Is this ever going to get any easier? What are we doing wrong?!
If you’ve read previous posts, you know that James has been in and out of the hospital several times for respiratory distress. We’ve been trying our best to care for him at home, but sometimes it feels like we’re not doing enough. We’ve been giving him breathing treatments at home. (Sometimes he even helps with his breathing treatments.) We were frequently suctioning his nose and mouth as much as needed and trying to manage his secretions the best that we could.

On Friday, February 26th, we took James to see the pediatrician again. We just couldn’t get his breathing under control and he had a little bit of a fever. Once again, the pediatrician had James admitted for respiratory distress.
They did a x-ray and ultrasound of his chest and he did not appear to have pneumonia. They did put him on an antibiotic, though, because of his fever.

An ENT (ear, nose, and throat doctor) came by to look at James and thought that overall he looked good. His only concern was to find a way to better manage James’ secretions. If we could find a way to manage the secretions better, maybe James wouldn’t have so many respiratory distress episodes.
James (and Stacy) only stayed in the hospital overnight and came home the following day.
]]>This poor kid (and his parents) just can’t catch a break. Here we go for another hospital stay. But before I get to that, I should probably fill you in with some back story in case you haven’t read the First Trip to the ER post. Even if you did read it, there is some additional information included here.
When James was in the hospital after Thanksgiving because of respiratory distress, another issue that James had was a very distended stomach. You can click on the link to read about stomach distension in depth if you wish, but in brief, James’ belly looked very bloated. At the time, the doctors thought that it was a result of James inhaling air into his stomach as he was gasping for breath because of the respiratory distress. They decided to stop his normal feeds and give him IV fluids until his respiratory issues improved. As his breathing got better, they slowly reintroduced his feeds. They took some x-rays just to be sure there wasn’t any sort of blockage, but everything looked fine from a gastrointestinal (GI) perspective.
That hospital stay was about ten days. After we got him home, we hoped things would go back to “normal”, but James was having some feeding issues. For some reason he would get cranky during his feeds and we didn’t know why.
We made it through Christmas without any issues other than the crankiness during feeds. We went to see the pediatrician the day after Christmas for routine vaccinations, and some blood work. On January 16, 2010 we took James to see a GI doctor that was recommended. We wanted to get a second opinion on some of the feeding issues that James was having. What a horrible experience that was! I won’t even try to sugar coat it.
It started off like any normal appointment when you see a doctor for the first time. We went over James’ medical history, the reason for our visit, and then the doctor a quick examination of James. This is where things started to go south.
When he was examining James’ belly, he pointed to the Mic-Key button and asked us what this was. Stacy and I just looked at each other with confused looks on our faces. I think we had the same thoughts going through our heads. “Did he really just ask that?” “Was he serious?” “Maybe he was joking.” “What kind of gastrointestinal doctor doesn’t know what a Mic-Key button is?” He then recommended that we get rid of the Mic-Key button and go back to a g-tube, which we took to mean the PEG tube like James had in the NICU before he got his Mic-Key button. Again, we looked at each other dumbfounded: “Did he really want us to go back to the PEG tube?” “Don’t the PEG tube and G-tube perform the same function?” “How could the Mic-Key button cause the feeding issues and why does he think the PEG tube was the answer?”
When we got in the car to go home, we confirmed that we both had the same questions going through our heads during the appointment. Neither one of us could figure out if the doctor was serious and didn’t know what a Mic-Key button was, or if he was trying to be funny. The fact that he questioned it without the slightest hint of a smirk lead us to believe that he really didn’t know what it was. Needless to say that was the last time we saw that doctor. He did prescribe a medicine that James was given when he was in the hospital that seemed to help with discomfort during feedings so we filled it and started giving it to James every 8 hours.
Two days after that appointment we noticed a yellow liquid was coming out of James’ g-tube so we went to see our pediatrician and he ended up having James admitted to the hospital. Not again! Fortunately, this hospital stay was only 3 days.
They did an upper GI with small bowel follow-through. For this test, they put some barium concoction into James’ stomach through his g-tube and watched how the barium moved through his gastrointestinal tract with a fluoroscope. Everything looked fine and things were flowing as they should.
Next they did an ultrasound of his abdomen and there was a concern about his gallbladder and wanted to another ultrasound in the morning. The follow-up ultrasound showed James had a stone in his gallbladder, but as long as it remained in the gallbladder it should not be causing him any pain. The stone would only be causing James pain if or when the stone gets lodged in the bile duct thereby blocking movement of bile from the gallbladder.
So after a couple of days in the hospital, and a few tests, we didn’t have any answers as to what was causing his discomfort with his feeds. James did have a few infantile spasms while in the hospital. We took a video of one episode and showed the GI doctor. Her opinion was that the spasms were a classic sign of reflux, put him on an anti-reflux medication, and proceeded to discharge James from the hospital. She didn’t feel like there was a need to keep him in the hospital, but did want us to follow up with her.
Side note: James did have what appeared to be seizures and infantile spasms while in the NICU and after we brought him home. This will be the subject of a future post. James also had a fundoplication procedure done while he was in the NICU which was supposed to stop reflux.

]]>
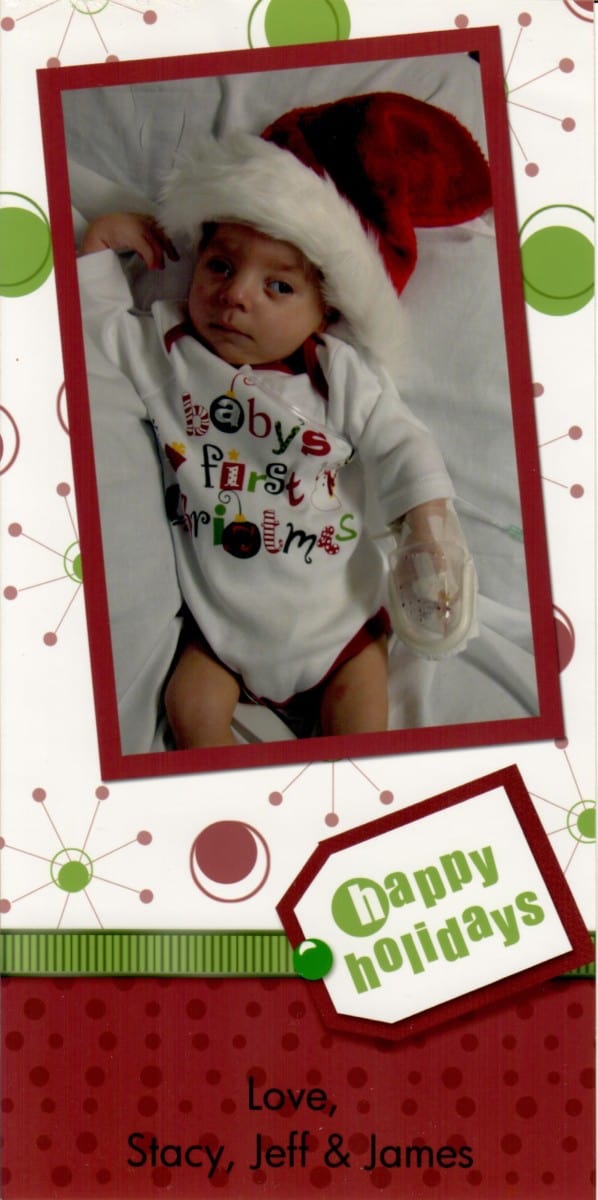
James’ First Christmas Card
How many of you send out picture cards for Christmas? This was something that Stacy and I started to do after we got married, and now it was James’ turn to take part in this tradition. Unfortunately, James ended up in the hospital shortly after Thanksgiving with respiratory issues so we weren’t able to take pictures of him by our Christmas tree like we wanted to. We ended up doing something a little bit different. Not wanting James to miss being on his first Christmas card, I went out, bought some garland and a Santa hat, and we tried to do a photo shoot in the hospital.
First we tried to pose him with the garland and Santa hat. This was probably the best of several pictures we took with the hat and garland:

Then we tried a couple of pics with the Santa hat and a mask to remind everyone to stay healthy. (This was during the H1N1 flu pandemic).

Then we tried posing James covered in the garland (with oxygen):

And another one without oxygen:

And then finally, we got a picture that Stacy and I both agreed was the best one for James’ first Christmas card:

Yep. That’s the one. Just James in his Santa hat. Simple.
James’ First Christmas
Because James came home from the hospital two weeks before Christmas, we decided to stay home for Christmas. We didn’t want to risk James getting sick again. Normally we would spend Christmas Eve at my mom’s with my side of the family and Christmas Day with Stacy’s side of the family. This year my Mom, sister and James’ cousin Sarah came over on Christmas Eve and Stacy’s parents came over on Christmas Day.
And we managed to get a pic of James by our Christmas tree:

The day after Thanksgiving (2009) James had an appointment with his pediatrician and got 3 vaccinations: Rotavirus, Hib (Haemophilus influenza type b) and IPV (Inactivated polio vaccine). By Saturday James had mucus constantly running out of his nose. For a while, we just couldn’t keep up with suctioning; it was just too much! We put James to bed around 9:00 pm with a little runny nose.
At 1:00 am Sunday morning Stacy got up to feed him as she normally did. She gave him a little suction in the nose and mouth and came back to bed. At 2:00 am she was up again to take down his feed. (Side note: this is one benefit of being tube fed. You can eat while you sleep!) James’ sats (oxygen saturation of the blood) were in the high 80s and low 90s. She tried to suction his nose and mouth, but was not getting much out. His sats were slowly dropping. By 5:30 am we decided to put him on a little bit of oxygen. (Because of his medical issues, we were provided with oxygen tanks from our home health provider.) Stacy went back to bed while I stayed up with him. When Stacy got up again at 10:30 am, we decided to call the pediatrician and take him to the ER.
One thing we learned pretty quick is that when you bring a baby into the ER on oxygen, you skip to the front of the line. We were immediately taken to a room where they started to assess him. Because he was in respiratory distress, they tried Atrovent, which is a bronchodilator that relaxes muscles in the airways and increases flow to the lungs. They took a chest x-ray which looked clear. Because of the H1N1 pandemic going on at the time, they tested James for the virus, but the preliminary results came back negative. They sent him up to the PICU (Pediatric Intensive Care Unit).
After further assessment in the PICU they thought James had a respiratory or viral infection and started him on an antibiotic, but was stopped because his blood panel came back normal. He had a fever so they gave him rectal Tylenol to try to bring it down. His stomach was very distended, so they used his g-tube and extension to relieve some of the air and gas that was built up in his belly from breathing so rapidly. They had him on up to 4 liters of oxygen trying to keep his sats up.
On Monday, James was given another chest x-ray and this one showed that he did develop pneumonia in the right lobe and was put on another antibiotic. He was given saline solution and Pedialyte because he was dehydrated. They did a renal ultrasound to see if his kidneys were working right and if there were any blockages because his blood pressure was so high. The ultrasound came back fine with no problems or obstructions. He tested positive for RSV, or Respiratory Syncytial Virus. According to WebMD, “Respiratory syncytial virus (RSV) is a common, and very contagious, virus that infects the respiratory tract of most children before their second birthday. For most babies and young children, the infection causes nothing more than a cold. But for a small percentage, infection with RSV can lead to serious, sometimes life-threatening problems such as pneumonia or bronchiolitis, an inflammation of the small airways of the lungs.” This really kind of pissed us off. Our pediatrician recommended a medication, palivizumab, that could have prevented RSV, but our insurance company denied it because he didn’t fit the criteria. We’re not really sure what that criteria is or if they just denied it because they were still trying to swallow the large bill from James’ two months in the NICU.
Because RSV is so contagious, James was put in isolation. Every time a nurse, doctor or anyone came into the room, they had to “suit up”. They had to put on disposable masks, and gowns before entering and thrown away upon leaving the room. We even got suited up while in his room.

James was put on diuretics hoping that they would force him to pee out any extra fluid in lungs or system. They were able to ween his oxygen down to between 1 and 2 liters, sometimes going as low as ½ liter, although he was still struggling to keep his sats up. They did a third x-ray in the evening which showed fluid and/or irritates in both lungs.
Our pediatrician stopped by on Tuesday and said that James had a rough night with his secretions. They will talk during rounds, but warned us that a tracheostomy conversation may be coming soon. (We had conversations about a tracheostomy (or trach for short) when James was in the NICU, because of his inability to suck or swallow.) The pediatrician also told us that he does not have RSV, but Enterovirus, which he described as a bad cold.
The PICU pediatric nephrologist (kidney doctor) ordered an ECHO of the heart to make sure it is pumping correctly because his blood pressure was so high, and also a kidney ultrasound. The results of both the ECHO and ultrasound were good. They did not see any problems with his heart or kidneys.
I could go on and on and cover everything that transpired over the course of his stay at the hospital, but that would make for a pretty long post and I don’t think too many of you would actually read it. So to summarize: The healthcare team went over all of James’ “problem areas” and all of the tests that were done and came up with a game plan. They decided to focus on fixing one thing at a time instead of trying to fix them all simultaneously. They were in agreement that the respiratory infection was the most serious so that would be the main focus. They also thought that the respiratory distress, which was causing him to gasp for air, was putting air into his stomach and causing his stomach to become distended. The hope was that once the pneumonia had cleared up and he was breathing better, James would not be sucking all the air into his belly. In the meantime, James would not be getting his normal feeds, but instead be given IV fluids to give him the nutrients he needed. They were also using his g-tube to relieve excess air and gas buildup in his stomach.
James (and Stacy) ended up staying in the hospital for about 10 days before he was able to come home. I went back to the NICU routine…driving 30 minutes to the hospital and 30 minutes back home every day. I had done this drive so much that I could probably do it with my eyes closed!
We knew when we brought him home from the NICU that things weren’t going to be easy. We were newbie parents to a cute little guy with several medical issues and we were still trying to navigate this new world that we were in. We were doing our best, and yet there we were, back at the same hospital that he had just come home from a month ago. Hopefully we can keep him healthy so we don’t wind up back at the hospital again.
One Final Note:
If you haven’t read about James’ Medical Binder, I encourage you to do so. A lot happened over the course of James’ 10 day stay at the hospital, and Stacy took notes that she eventually typed up and put into the binder. I don’t know about you, but I have a pretty bad memory. By having written notes, you won’t forget everything that happened in the hospital, what tests were done, what the test results were, what medications were given, what doctors were involved, etc. If you don’t have a notebook with you, use a notes app on your phone or tablet if you have it with you. Or ask a nurse for some paper and a pen.
]]>Thanksgiving is probably one of my favorite holidays. It’s a time to get together with family. A time to reflect on the past year and think about the things you are thankful for. Maybe watch some football. And my favorite part? The food! You probably couldn’t tell by looking at me that I love to eat. I am one of the fortunate ones that was blessed with a fast metabolism. At least I was. As I have gotten older my metabolism has slowed down a bit so I’ve been a little more conscious of what I eat, but Thanksgiving will always be the one day a year that I eat until I feel like I’m going to split my pants. Christmas comes in a close second.
Thanksgiving 2008 was a very hard and emotional Thanksgiving for us. We had lost Jackson just 10 days before. Trying to be thankful when your first child passed away before he was born was a struggle. Of course we were thankful for our health, and the health of parents and siblings. But the pain, the anger, the helplessness, the emptiness, and the depression of losing Jackson were still overwhelming.
Fast forward a year and we were blessed with James. We had so much to be thankful for this year. We hadn’t forgotten about Jackson, and we never will. He will always be considered our first child. Having James made Thanksgiving 2009 much more bearable. Sure James was disabled and required around-the- clock care, but he was ours. He made us a family.
When Stacy and I got married, we went through all of the major holidays and figured out which holiday would be spent with which side of the family. Thanksgiving was spend with her side of the family so we packed up our little car and headed off to her parents. Thanksgiving itself was pretty uneventful. Lots of good food, football, family. Just a typical Thanksgiving. And of course I ate too much!
James is still new to us and we’re still trying to figure him out. He’s kind of like a puzzle with missing pieces. He has neurological impairments so we’re not sure what he understands. He has vision issues with an optic nerve that wasn’t fully developed so we are not sure what he sees. He might have hearing issues so we are not sure what he hears. None of this is going to stop us from trying to give him all of the life experiences we can. We’re not sure if he enjoyed his first Thanksgiving or not. We didn’t hear any complaints, so I guess that is a good sign. To be fair, though, James isn’t much of a complainer. He doesn’t cry much, which we think is a result of his neurological issues.
We brought James home from the NICU on October 29th, just in time for Halloween. We knew James was not “normal”, but we didn’t want his disabilities and medical issues to keep him from experiencing life. What is “normal” anyway? Dictionary.com defines normal as:
- conforming to the standard or the common type; usual; not abnormal; regular; natural.
- serving to establish a standard.
- Psychology
- approximately average in any physical trait, and intelligence, personality, or emotional adjustment.
- free from any mental disorder; sane.
- Biology, Medicine/Medical
- free from any infection or other form of disease or malformation, or from experimental therapy or manipulation.
- of natural occurrence
One of the above definitions of normal is “free from any infection or other form of disease or malformation”. Okay, so maybe James isn’t what most people would consider normal. But does it matter? It didn’t matter to us. We weren’t going to keep him in a bubble for his entire life. When he was in the NICU there were questions about what his quality of life was going to be. And there were questions about how long he would live with all of his medical issues. We wanted him to experience as much as he could in his life, however long or short it may be.
Since James came home from the hospital two days before Halloween, we didn’t waste any time giving him one of his first life experiences…we got him dressed up for Halloween. We didn’t take him Trick or Treating, though. We took James to Nana and Papa’s (Stacy’s parents) house, so he could hang out with his cousins.
Stacy has always had a thing for Tigger from “Winnie-the-Pooh” so it was fitting that James’ first Halloween costume was Tigger. James actually wore two outfits for Halloween. He rode to Nana and Papa’s house in a “My First Halloween” onesie and then changed into his Tigger costume.


I’m sure you’re wondering what the wires are coming out of the top of the Tigger costume. The gray wire goes to his sleep apnea monitor, in case he stops breathing in his sleep. The leads for the monitor are attached on his chest. We had a love / hate relationship with the sleep apnea monitor. More hate than love I think. It was constantly giving false alarms. The white wire is for his pulse ox that monitors the oxygen in his blood as well as his heart rate. The probe for the pulse ox is wrapped around one of his toes. With the pulse ox we were more concerned with his oxygen levels than his heart rate because of his inability to swallow his secretions and needing frequent suctioning.
One thing we learned from putting him in his Tigger costume is that one piece outfits that zip all the way up and have footies do not work well for James. The wires for his sleep apnea monitor and pulse ox were one issue. We had to route the wires out the top of the costume. He is also g-tube fed so in order to feed him, we had to unzip the costume.
I think James had a good first Halloween. He was only two-months old so I doubt he remembers it. He slept through most of it anyway. But we have the cutest pictures to show him when he gets older!
]]>

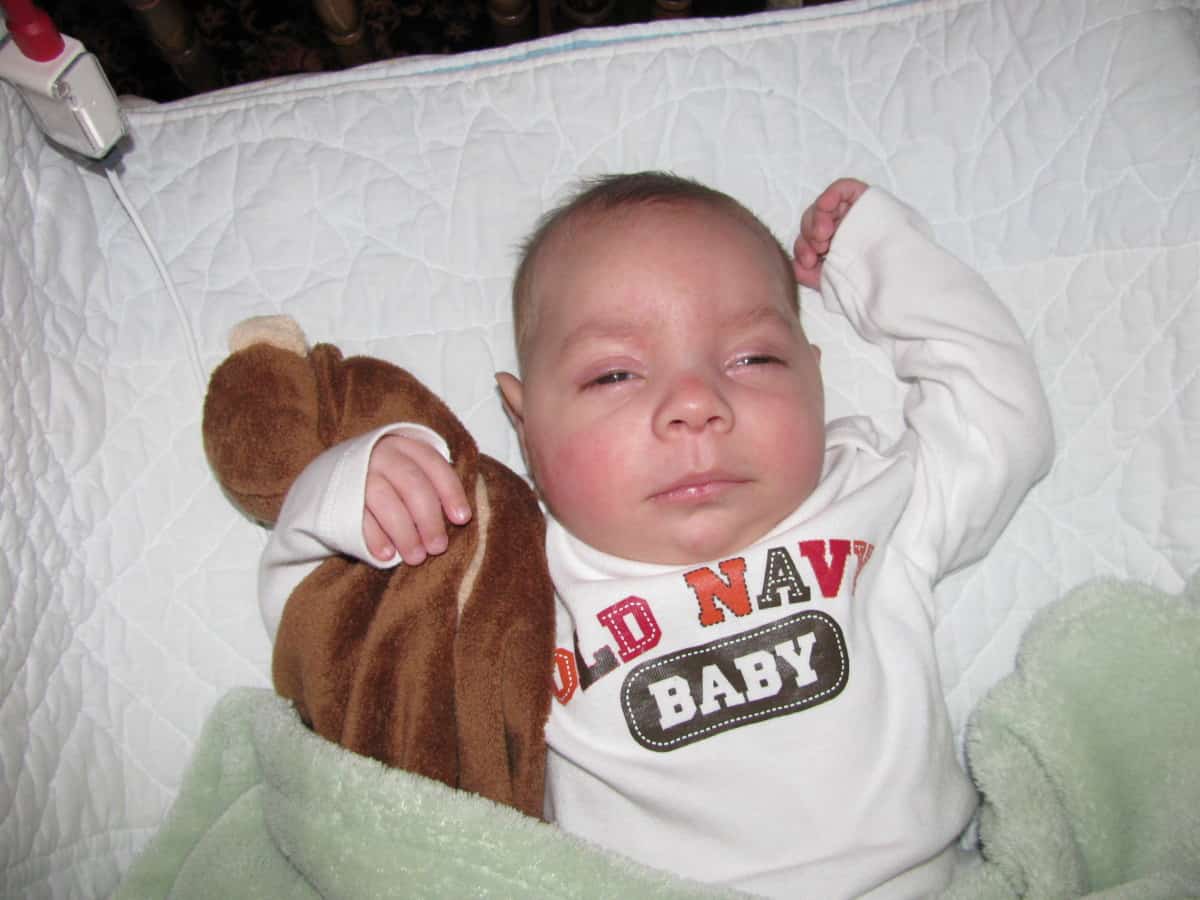
There’s James…all tucked into his bed in his room at home. After 2 long months in the NICU, he finally came home on October 29th, 2009. I’ve heard enough stories that to know that new parents go through an adjustment period when they bring home their healthy new baby. We don’t know what that adjustment period is like because we have never had the opportunity to bring home a healthy baby. Jackson passed away before he was born and James, well, he came home with things that most parents don’t have to deal with.
There was the feeding pump that is used to pump his food (breast milk, formula, or Pedialyte) through his g-tube and into his stomach. There was the pulse oximeter (pulse ox) that constantly monitors his heart rate and the oxygen levels in his blood. There was the suction machine that we use to clear the secretions from his nose, mouth and throat because he is unable to do it on his own. There was a sleep apnea monitor just in case he stopped breathing in the middle of the night. There were oxygen tanks in case he needed a little boost like he did on several occasions in the hospital. And there were the prescription meds he was taking. “Are we sure we can handle this?” Well, we didn’t exactly have a choice, did we? Welcome to our new normal.
During the two months that James was in the NICU, we were there as often as we could be so we knew what his care was going to be like once we got him home. But there’s one big difference between the hospital and home. In the NICU there were nurses tending to him around the clock. Now that he’s home, it’s just Stacy and I. The two of us were responsible for little person with so many medical issues. Deep breaths. We got this! Welcome to our new normal.
When James was in the hospital, they had him on a schedule. He was getting fed every three hours. He was getting his meds at specific times. We continued this schedule at home. It was rough, but we managed to get through it. Actually, I think Stacy did most of the managing. You see, I am a heavy sleeper and can sleep through just about anything. Stacy, on the other hand, can wake up to the sound of a pin dropping on a tile floor. Alright, maybe not that bad, but she is a pretty light sleeper. James doesn’t cry, so we didn’t have to worry about him crying us…I mean Stacy… awake all night. Instead, we had the lovely sounds of his pulse ox and sleep apnea monitors beeping randomly throughout the night. Have you ever walked through a hospital and heard machines or monitors beeping as you passed by a patient’s room? Now imagine that beeping coming from your child’s room at all hours of the night. After two months in the NICU we kinda got used to a nurse rushing over to James if one of his alarms went off. We quickly realized that this isn’t the hospital. There are no nurses here. There was just me and Stacy taking turns to tend to James.
Welcome to our new normal.
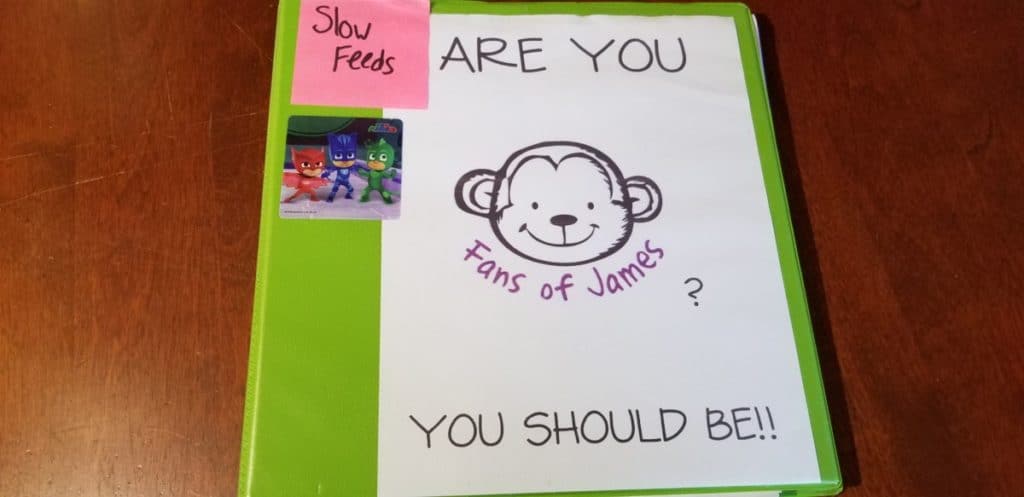
When you have a “normal” kid, you keep track of the usual things: height, weight, and vaccinations. Pretty easy, right? Things are a bit more complicated when you have a child with disabilities or medical issues. When James was in the NICU, Stacy started jotting down notes in a notebook. These notes included doctor’s and nurse’s names; any tests or scans that were done; any tests or scans that were requested, but not yet performed; surgeries; any thoughts or questions we wanted to discuss with a doctor or nurse; etc. Anything pertaining to James’ medical care was noted in the notebook. These notes were eventually typed up into a Word document and became the start of what is now James’ medical binder. We refer to it as the “James Bible”. It includes all of James’ medical info and it’s one of the main things we grab when we go to the hospital, either for a scheduled surgery or procedure, or if we have to rush him to the Emergency Room. I encourage anyone who has a medically compromised child to start a binder of their own. Depending on how medically challenged your child is, there might be a lot of things to remember, and you can’t remember everything. It will become an invaluable reference. This is how we have put together James’ binder. You might opt to do it differently, but this will hopefully give you an outline of what should be included.
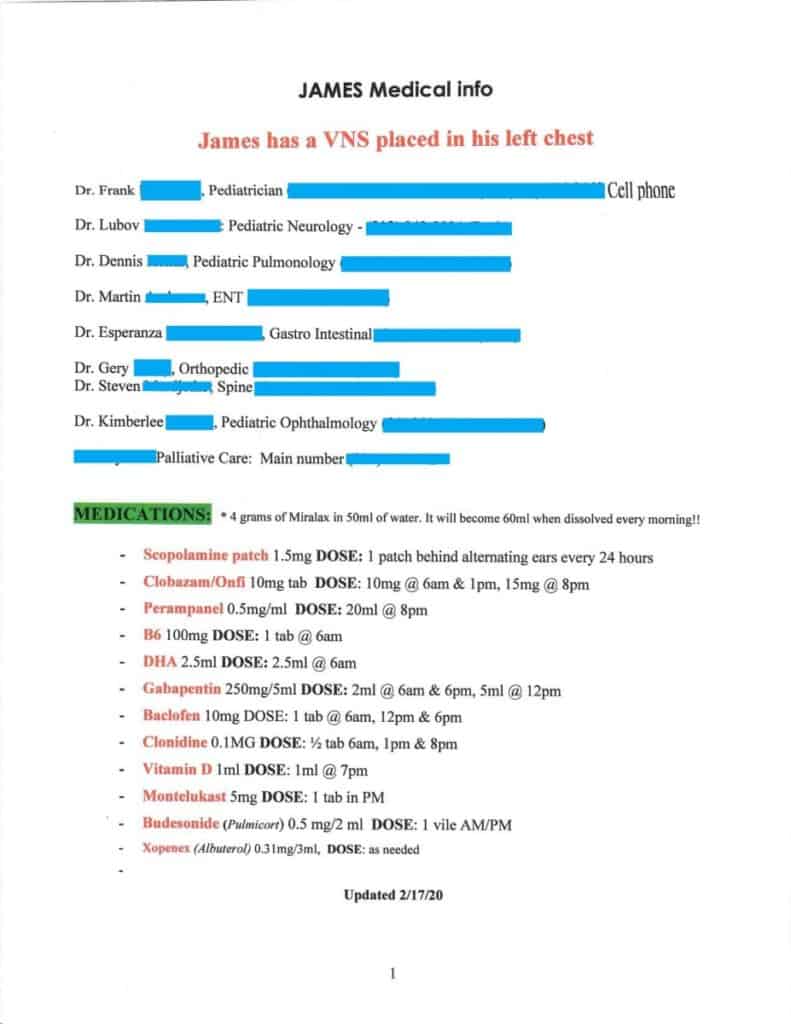
Doctors and Medications
A list of James’ doctors (with their phone numbers) and current medications is the first thing you see when you open the binder. This is extremely handy when he goes to a doctor or to the Emergency Room. They always ask about any medications he is on. We just pull out the sheet for them to look at or make a copy of. Note the date at the bottom of the sheet. This is important because medications and dosages are can change from time to time. You want to give medical staff the most recent list of medications.
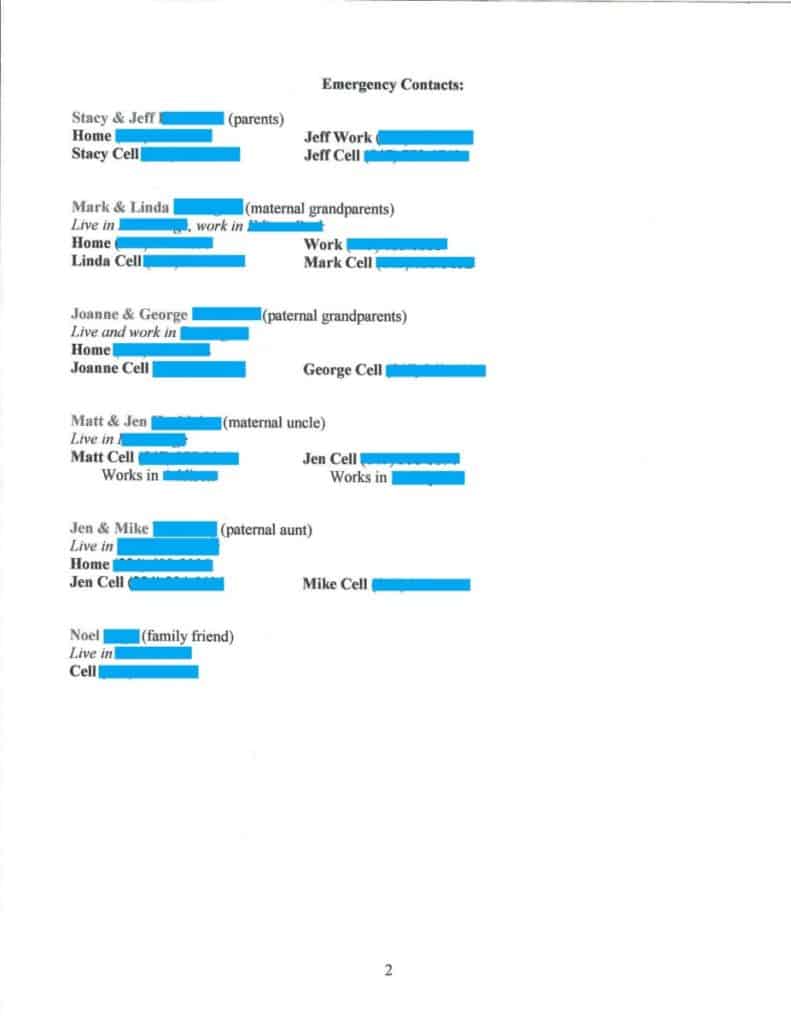
Emergency Contacts
Behind the list of doctors and medications is a list of emergency contacts. This includes our home, cell, and work numbers as well as phone numbers for immediate family and their relation to James.
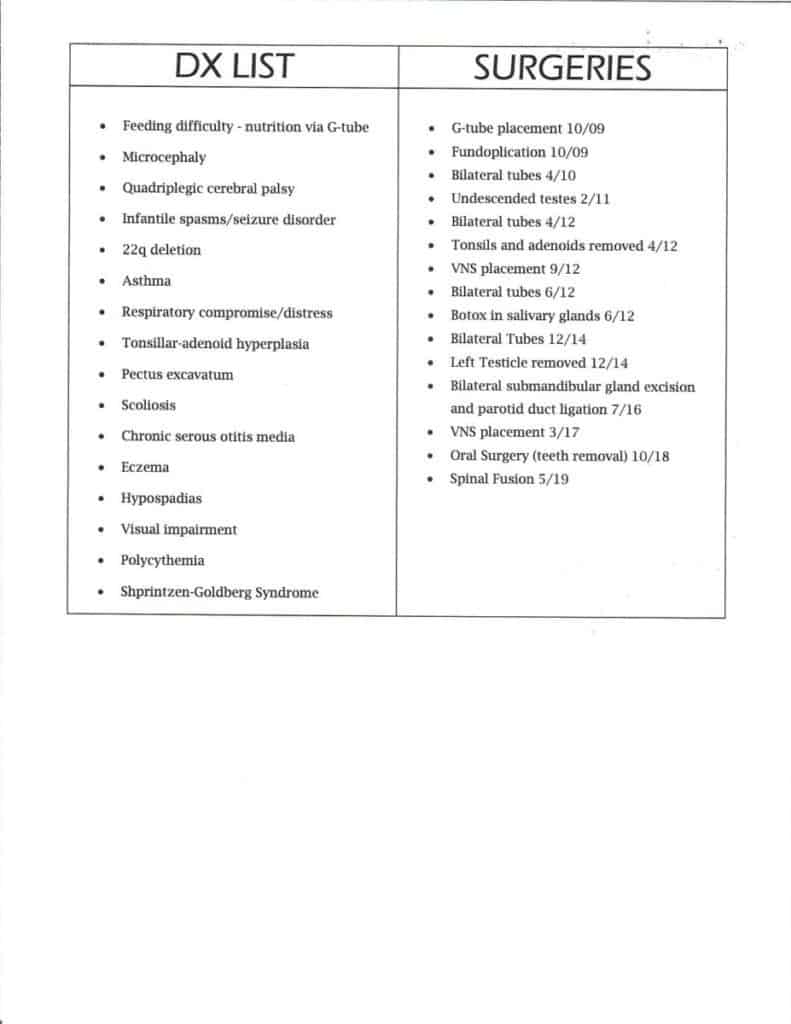
Diagnoses and Surgeries
Next up we have the list of diagnoses (DX) and surgeries. Next to the surgeries we have the month and year the surgery was performed.
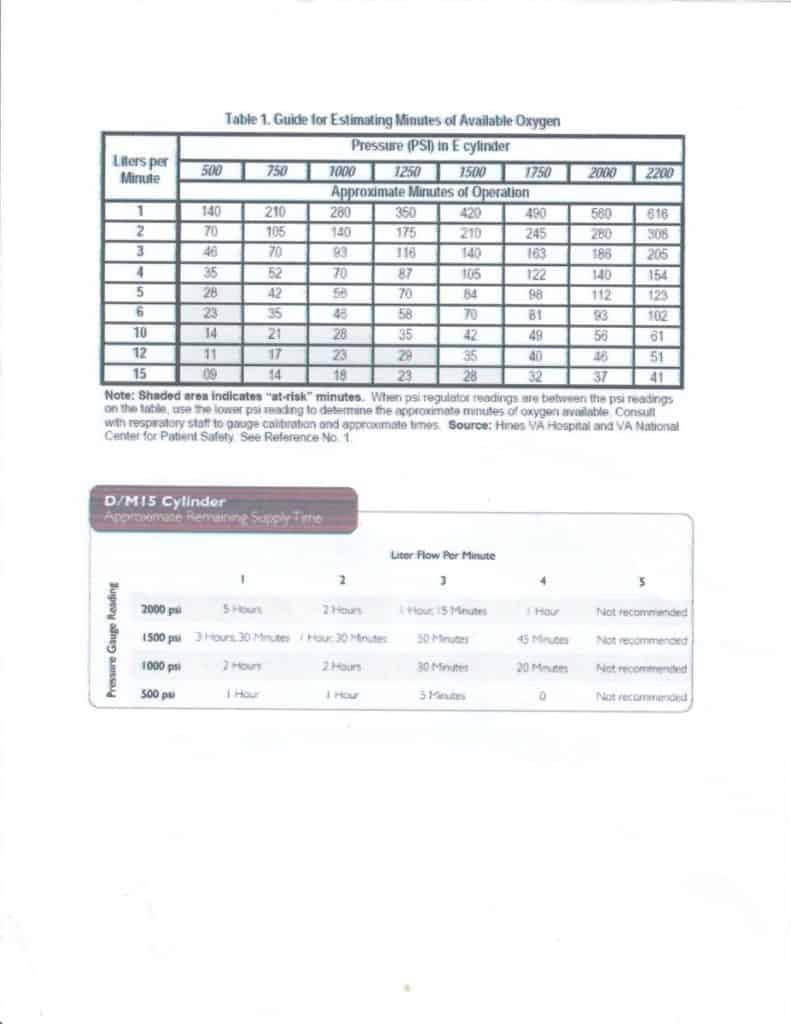
Oxygen Chart
Because James has occasional respiratory distress due to his inability to clear his own secretions, we have oxygen tanks in the house so included in his binder is a “Guide for Estimating Minutes of Available Oxygen” chart. There are many different sizes of oxygen tanks and each size will have a different chart. At one point we had both E cylinders and D cylinders, so I found charts online for each of those sizes, and copied them onto a Word document so that we could have one page that had both charts. The E cylinders are big and not very portable. Now that we have an oxygen concentrator at home, we rarely use them. The D cylinder is smaller and much easier to travel with. James has one on his wheelchair, so it is with him at all times. Although the 2 charts below are laid out a little differently, they tell the same information. The two numbers you need to be concerned with are the pressure (PSI) and the liters per minute. The pressure you will find on the gauge attached to the tank. This is how much oxygen is left in the tank. The less oxygen there is in the tank, the lower the pressure will be. The liters per minute is on the regulator that you can adjust. Once you know those two numbers, you can look at the appropriate chart for the oxygen tank you have and get an estimate of how long you have before the tank is empty. If you have any questions regarding any oxygen tanks you may have, please contact your home health provider.
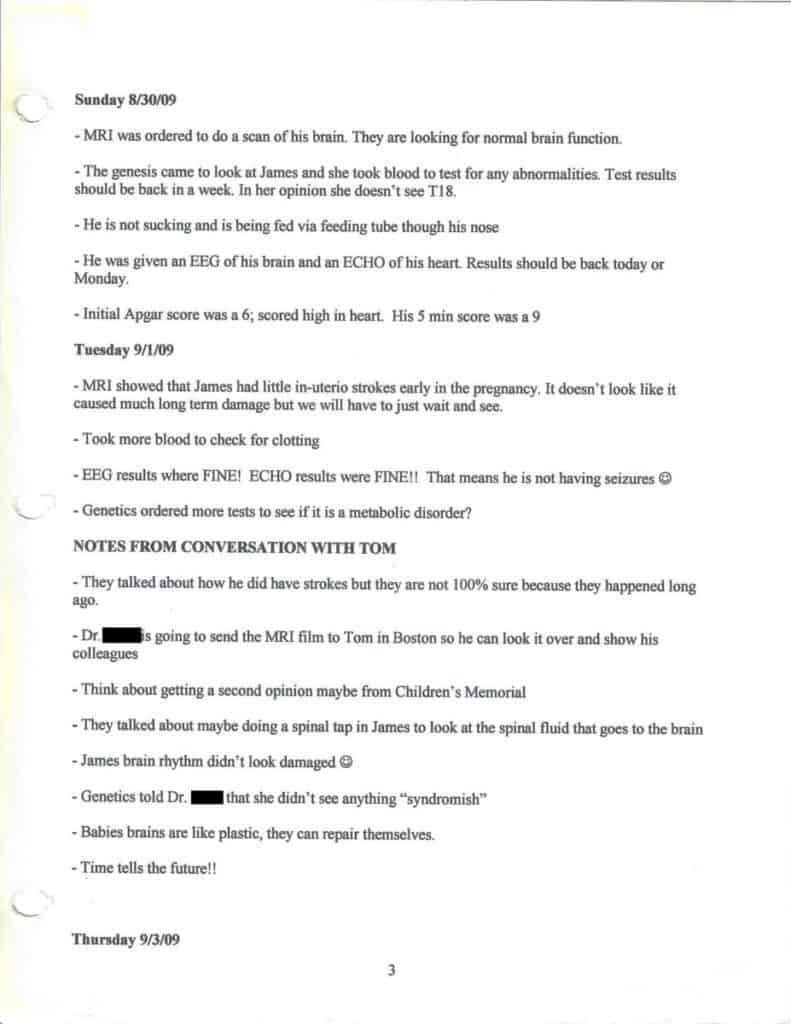
Blank Notebook Paper
Also included in the binder are blank pieces of notebook paper. These are for jotting down quick notes when you are talking to a doctor or nurse. These also come in handy if you have a question you want to ask a doctor or nurse next time they come into your hospital room.
When you have some free time, I recommend that you take your notes and type them up into a Word document. This not only makes it easier for others to read, but it also makes it easier to find something specific. Instead of skimming through a bunch of handwritten notes, you can just open the Word document and use the search feature. Here is an example of some of our notes from James’ first couple of days in the NICU:
Other Things Included in the Binder
Also included in our binder are:
- Any of James’ charts or notes that we may have received from a doctor
- Doctor’s business cards
- Extra pens and pencils
Summary
So that’s James’ “Bible” in a nut shell. If you’re child is as complicated as James is, I highly recommend you put together a binder like this. It is an invaluable tool. Stacy takes James to most of his appointments and stays at the hospital with him whenever he is admitted. I try to be involved as much as I can with his medical care, but if it wasn’t for his medical binder, I would be lost. Besides, I sometimes can’t remember what day it is, let alone when James had X surgery or what his dose of Y medicine is.
]]>James was born full term at 12:30 am on August 29, 2009. The pregnancy was uneventful without any complications or surprises like our previous pregnancy. (Please refer to The First Pregnancy section of Our Story to learn more about the previous pregnancy). We went to all the prenatal doctor appointments and everything about this baby, who we would later name James, appeared to be normal. We thought we were having a normal, healthy baby boy. With the pain and heartbreak of losing Jackson, this was such a relief. It wasn’t until Stacy’s water broke on August 28th that we knew something wasn’t right.
After her water broke, Stacy quickly ran to the bathroom to clean up while I started to get things ready to go to the hospital. As Stacy was cleaning herself up, she noticed what appeared to me meconium in the amniotic fluid. Meconium is a babies first stool and contains materials ingested by the fetus within the womb. It is usually passed in the first few hours or days after birth. When meconium is passed prior to birth, it can make it harder for the baby to breathe because it can clog the airways, irritate the airways and injure the lung tissue, and block surfactant, which is a fatty substance that helps open the lungs after birth. (The preceding information about meconium was taken from https://kidshealth.org/.)
We rushed to the hospital (which was a 30-minute drive) as fast as we could. When we got to the hospital, we were taken to labor and delivery and the nurses started the routine pre-delivery prep work. There was some concern that James wasn’t moving. One of the nurses reached up inside of Stacy to try to attach some probes or something and when she lightly scratched his head, he still didn’t move. She feared that he was in distress and called for an emergency C-section. I can’t explain what we were feeling at that moment. We were in utter disbelief. How did we go from the Jackson pregnancy where we knew something was wrong early on, to this pregnancy where everything seemed normal, only to be thrown this curveball? “Was James okay?” “Please be okay!” “God, please don’t do this!”
When our OBGYN on-call arrived, Stacy was wheeled into delivery to get James out as quickly as possible. At 12:30 am on August 29th, James was brought into the world. I had seen enough movies and hospital shows to know that a baby cries shortly after birth, but James didn’t cry. As we held our breathes waiting for him to cry, we were told that he was alive, but they weren’t sure what was wrong, so they were going to take him to the NICU for further observation and testing. The NICU, or Neonatal Intensive Care Unit, is similar to an Intensive Care Unit (ICU) for adults, but the NICU is for babies. Babies that are born premature, who have had a difficult birth, or who have health problems are sent to the NICU. There they receive around the clock care by a team of nurses, doctors, and specialists. We were fortunate enough that James was born in a hospital with one of the best NICUs in the area. If you want to read more about what a NICU is, please visit this page: https://kidshealth.org/.
Before I continue with our experience in the NICU, I thought I would take a moment to explain what a NICU is, for those of you who don’t know what it is, have never been in one, or happened to stumble across this page because your little one was recently admitted to the NICU and are Googling for information.
What is a NICU?
NICU stands for Neonatal Intensive Care Unit, or sometimes called Newborn Intensive Care Unit. Similar to an Intensive Care Unit (ICU) for adults, a NICU is a special unit a hospital for babies that are born premature or are born with serious medical issues. A NICU has advanced technology and is staffed by highly trained healthcare professionals to give special care to the tiniest of patients.
Do All Hospitals Have NICUs?
Unfortunately, not all hospitals have NICUs. We were lucky that James was born in a hospital with a Level III NICU. If the hospital didn’t have a NICU, he would more than likely have been transferred to a hospital that did, either by ambulance or helicopter. Babies who need intensive care after birth do better if they are born in a hospital with an NICU than if they are moved after birth (https://www.stanfordchildrens.org). For this reason, if you know that your baby has a medical condition before birth, it is recommended to give birth in a hospital that has a NICU, if possible. Of course, medical conditions may not be known prior to birth. We had no idea that James had so many medical issues before he was born.
Are All NICUs the Same?
Before James was born, I had very little knowledge of what a NICU was. We did a Labor and Delivery tour at the hospital during the pregnancy, but the NICU was not included on that tour. About all I knew about a NICU was that preemies went there and were placed in incubators to keep them warm. It wasn’t until after James was admitted to the NICU that I learned more about them and that there are different levels of NICUs. According to the March of Dimes, there are 4 levels of medical care for babies. They also note that babies can move from one level of care to another—to a higher level if they need more care or to a lower level as they get better and are ready to go home.
- Level I – Well Newborn Nursery
- This kind of nursery has a clinical team of health care providers who take care of:
- Babies born on time (at about 40 weeks) who are stable (for example, they can breathe on their own and can maintain their body temperature)
- Babies born at 35 to 37 weeks who are stable
- Babies who are sick or born before 35 weeks, but only until they can be moved to a nursery with a higher level of care
- This kind of nursery has a clinical team of health care providers who take care of:
- Level II—Special Care Nursery
- This kind of nursery has a clinical team who takes care of:
- Babies born at or after 32 weeks who weigh more than 1,500 grams (3.3 pounds). These babies may have some health problems, but they’re not so serious that they need a higher level of care.
- Babies born before 32 weeks or less than 1,500 grams, but only before being moved to a higher level of care.
- Babies who have just gotten out of a newborn intensive care unit (also called NICU) and are growing and doing well before being able to go home.
- Babies who need equipment to help them breathe. These babies should stay in this kind of nursery only for about 24 hours or less; if they need breathing help longer, they should be moved to a higher level of care.
- Level III, NICU
- This kind of nursery has a clinical team who takes care of:
- Babies born before 32 weeks who weigh less than 1,500 grams.
- Babies of any age or weight who are critically ill.
- Babies who need equipment to help them breathe to stay alive.
- This kind of nursery has a clinical team who takes care of:
- This kind of nursery has a clinical team who takes care of:
- Level IV, Regional NICU
- This is the highest level of care for babies. This kind of nursery has a clinical team who takes care of babies who need special surgery for birth defects and other disorders. This nursery has a full range of health care providers, including pediatric subspecialists, specialized nurses and equipment to care for very sick babies.
What’s It Like in the NICU?
Now that I have explained a little bit about what a NICU is, I’ll continue with our experience. The first time we went to see James in the NICU, we were scared and nervous. We didn’t know what to expect. All we knew about James at that point was that he had some issues that were a bit concerning, but didn’t know to what extent. I saw him only for a few seconds after the delivery; Stacy didn’t see him at all. He was quickly tended to by the nurses and whisked away to the NICU, so this would be our first time officially meeting our son. We were escorted down to the NICU from our room on the Labor and Delivery floor by a nurse. When we got to the NICU, we had to sign in and had to be buzzed into the unit. We would have to do this each time we went to visit. Once inside the unit, we were escorted to Pod D. Easy to remember, because it sounds like “potty”. Anyway, the NICU at our hospital had several rooms that they called pods. I’m not sure if each room (or pod) was set up the same way, but Pod D had 10 tiny beds in it, five on each side, with an open walkway down the middle. James’ bed was the first one on the right-hand side of the room.
Once we were in James’ pod, we were greeted by a nurse who was on shift in the pod. She went over the preliminary findings, what the concerns were, which doctors and specialists had seen him already, and which ones they were still waiting for. James would spend the first two months of his life in this room. By the time we were able to take him home, we had a lot of answers as to what was wrong with him. One of the things that Stacy started doing pretty much right away was taking notes in a notebook…doctors names, nurses names, any tests that were ordered, any questions we had, etc. These notes were eventually typed up into a Word document and became the start of what is now James’ medical binder. We refer to as the James Bible. I encourage anyone who has a medically compromised child to start a binder of their own. You can’t remember everything and it will become an invaluable reference. To learn more about James medical binder, click here.
As I mentioned previously, James spent his first two months in the NICU. As a matter of fact, it was exactly two months. He was born on August 29th, and went home on October 29th. As you will see below, a lot happened over those two months, which is why it it a good idea to get a notebook and take notes. I have included all of Stacy’s notes here. Please note that although our documents include doctor’s and nurse’s names, I have removed them here and just use their specialty, for privacy reasons. I don’t expect you to read all of the notes. You can skim through them if you wish. There is a pic of James on his way home, a few final thoughts, and a synopsis of all of the medical issues that were found while James was in the NICU at the bottom of this post, so be sure to scroll all the way to the bottom so you don’t miss anything.
Sunday 8/30/09
- MRI was ordered to do a scan of his brain. They are looking for normal brain function.
- The geneticist came to look at James and she took blood to test for any abnormalities. Test results should be back in a week. In her opinion she doesn’t see T18.
- He is not sucking and is being fed via feeding tube though his nose.
- He was given an EEG of his brain and an ECHO of his heart. Results should be back today or Monday.
- Initial Apgar score was a 6; scored high in heart. His 5 min score was a 9
Tuesday 9/1/09
- MRI showed that James had little in-uterio strokes early in the pregnancy. It doesn’t look like it caused much long term damage but we will have to just wait and see.
- Took more blood to check for clotting.
- EEG results where FINE! ECHO results were FINE!! That means he is not having seizures.
- Genetics ordered more tests to see if it is a metabolic disorder?
NOTES FROM CONVERSATION WITH {Stacy’s Dad’s cousin}
-
- They talked about how he did have strokes but they are not 100% sure because they happened long ago.
- Neurologist is going to send the MRI film to Dad’s cousin in Boston so he can look it over and show his colleagues.
- Think about getting a second opinion maybe from Children’s Memorial
- They talked about maybe doing a spinal tap in James to look at the spinal fluid that goes to the brain
- James brain rhythm didn’t look damaged
- Genetics told Neurologist that she didn’t see anything “syndromish”
- Babies brains are like plastic, they can repair themselves.
- Time tells the future!!
Thursday 9/3/09
- 7:30am phone call from NICU Pediatrician:
- James started breathing heavy in the middle of the night so they called for a chest x-ray to see what was going on. They found a little spot on the top of his RT lung that they believe is pneumonia. He was aspirating on his feedings so they stopped feeding and is now being given antibiotics to fight the pneumonia.
- 9:30am phone call from a nurse:
- She called to get permission to insert a PICC line (peripherally inserted central catheter) into his arm that will go into his chest. He will receive IV fluids via line and maybe feedings and antibiotics at a later date. This will be inserted only in the NICU and will be removed once he can tolerate feedings. ** 1:35pm x-ray for PICC placement. It took 3 tries
- Speech did come to see him today we will be awaiting results of that assessment.
- I did speak to NICU to schedule a family meeting with neurology, genetics, and NICU attending. There will be other professionals attending this meeting as well.
- Ophthalmology came to assess him. Eye Doctor dilated his eyes and assessed them. The right eye looks good but the left eye’s optical nerve is not fully developed.
Friday 9/4/09
- Today he was pricked to give blood to test his gases and he flinched and kicked the nurse a bit. He didn’t like that and to us that shows that he has feeling in his limbs and telling us. He was also squeezing Jeff’s finger while getting his blood drawn.
- Gases came back fine.
- He also let out cry today. Jeff, the nurse and I were all in shock!!
Saturday 9/5/09
- Nurse came to talk to us about the spinal tap results. She said the preliminary tests came back fine but the real in dept test is still out. We should have results soon!
- Nurse talked about Factor V and if it is Heterozygous or Homozygous.
Sunday 9/6/09
- Today I got to kangaroo him and he seemed to enjoy the feeling of mom’s touch on his body.
- Got a bath and weighed at night, he is 6lb and 5oz now. Gaining little by little.
- I saw him trying to move his tongue today around 9:50pm. He was also keeping his mouth closed more while he was sleeping. He might be a mouth breather; I know that I would be with all those tubes in his nose!
Monday 9/7/09
- He will receive his CRP tests in the morning. This is used to check for infection. He was high a few days ago that is why he was put on antibiotics, was rechecked on 9/6 and he was low
- Reintroducing breast milk, 10cc over an hour.
- Pediatric Hematologist will talk to us about possibly getting tested for Factor V
Tuesday 9/8/09
- James had a rough night last night. He had 3 or 4 spells where his saturation got low. He was bumped up to 60 in his oxygen to help him get his numbers back down. They ordered an EEG at 9am to see if he was having seizures but no news is good news! Nurse was Sarah.
- SPL came to see him today and worked on his oral motor skills. She told the nurse that they are not going to cut his tongue yet because it might cause his tongue to go backwards into his throat.
- The Occupational Therapist (OT) came in while we were there. She showed us some simple moves to work on when we are there. She was getting him to relaxed he kept letting out little sighs and became very relaxed.
- They are bumping his feeds up to 15cc over a 2 hour span. He is keeping his feeds down and they are coming out into his diaper so we know he is digesting his meals.
- They are looking into maybe reducing his oxygen and maybe trying real air for a bit and see how he does with that.
Wednesday 9/9/09
- He is off the oxygen!!
- At night the nurse didn’t clean out his tube to see how much residual came back up. She also ALMOST gave him 50ml instead of 15 because she thought the nurse before her said 50. I caught it before he got too much.
Thursday 9/10/09
- Still getting 15ml of milk but this time over a span of 3 hours. The overnight nurse said that she was suctioning him a little bit more than usual and some of it was milk.
- I did speak with the charge nurse about the incident with milk and she said she will speak to that nurse and not place her with him anymore.
- Our family meeting is Friday @ 8:30am.
- Speech came today, missed her AGAIN! I think I will have to place a call to her and make sure that our paths do cross and I can learn some stuff from her.
- My dad spoke with his cousin tonight and he said to make sure to touch James’ legs, arms, face, body and do that for about 10 minutes about 3-4 times a day. Make sure he knows that these are his body parts and this is how they move.
Friday 9/11/09
- Family meeting notes:
- The 2 vessel cord has nothing to do with his situation, neither is the Factor V Leiden or when I had my fever.
- The lack of movement when he was inside probably means that he might not be able to move on his own later on in life. We will have to wait and see.
- Tone abnormalities: hypertonic legs (tight) and hypotonic trunk (low)
- MRI saw damage on the white matter of the brain, the “wires”. The abnormalities are localized to certain areas of the brain and we don’t know what is affected by those abnormalities.
- They sent blood to test for Lukodystphy; rare by serious disability.
- His chromosomes came back normal.
- Palative care would come in to help us with transitions and whatever we would need from the hospital.
- Speech Language Pathologist came in to work with him. I got to see how so strokes his cheek while he is eating to stimulate the face muscles and associate them with eating. She also strokes his lips and then goes into his mouth the strokes the roof of his mouth. Today when she did that, he closed his lips around her finger and moved his tongue a little bit. WHOO HOO!!
- Physical Therapist came today as well. She showed me some arm and leg movements to open up his limbs and get him lose.
- Night nurse said she was going to try to shorten his feeding time from 3 hours to 2 ½.
Saturday 9/12/09
- They stopped feeding him my milk. He was having difficulty keeping his sats up and food down.
- Geneticist took more blood and sent it off for lysosomal enzyme testing.
- Finished his antibiotics @ 10pm.
- Slept good they said.
Sunday 9/13/09
- Still on the IV for feedings. Hopefully will try again Monday but I don’t see hope that he will keep it down. He is making so many secretions and is getting suctioned every hour sometimes more than once.
- They did a chest x-ray to see about the pneumonia and it came back cloudy so they are giving him antibiotics again. They also took blood to test (CRP) and if they see an infection they will continue the antibiotics, if they don’t then they will stop the antibiotics.
- We spoke with nurse and she was saying that since he has no gag reflex we don’t see bottle feeding happening anytime in the future. His future is looking more towards a g-tube every day.
Monday 9/14/09
- He is on antibiotics: Piperacillin/Zosyn & Vancomycin
- Still on Oxygen, very low
- Started taking Pepcid for his acid reflux
Tuesday 9/15/09
- Stopped taking the antibiotics.
- 8am he was off oxygen but back on very low to get him through the night around 8pm.
- Taking Reglan to help his GI track more quickly and freely.
- Taking 10ml of breast milk again… little by little he will hopefully work up a tolerance for it and keep it down.
Wednesday 9/16/09
- Infectious disease doctor came to look over James and everything looks good.
- 15ml of milk over 3 hours.
Thursday 9/17/09
- OT came to see him and work on his swallowing. She was trying to work his throat muscles to strengthen them.
- 20ml of milk over 3 hours.
Friday 9/18/09
- Long chain fatty acid test came back normal; NO adrenal leukodystrophy.
- Organic acid & amino acid tests came back normal.
- 20ml over 3 hours still.
- Speech Language Pathologist came to work with his oral motor. She created a great deal of secretions and you could tell he was working on clearing them by himself a little bit. He did need to be suctioned but he was trying.
- Physical Therapist came and showed me more PT moves while he is lying on his belly. She will come back with pictures and mini write up on what to do.
- Pepcid – every 12 hours and Reglan- every 6 hours. Keeping 20ml for a while longer don’t want to push him to much.
- Monday they are sending more blood to run a lysosomal enzyme test and the microarray test. These are deeper chromosome tests, non specific. Could take 4 weeks but she is on the team that does the tests so as soon as she knows she will tell us.
- Friday (5pm) they put in a NG (nasogastric) and NJ (nasojejunal) tubes for his feeding. Took a few attempts.
Saturday 9/19/09
- The NG and NJ tubes are in. He gets his meds via NG and his feeds via NJ. He is getting 25ml of milk over 3 hours.
Sunday 9/20/09
- He is getting 35ml of milk over 3 hours.
- 7lbs and 9 oz.
Monday 9/21/09
- They are going to keep his feeds at 40ml over 3 hours.
- There was talk over rounds about stopping the Raglan for 3 days and perform an upper GI on Friday to see where how much acid is in his stomach and how much is refluxing.
- Once they get the results of the upper GI they will discuss performing a Fundoplication to keep the acid down. Jeff and I are not sure if we want to do this or not. We will have to talk it over with a GI doc.
- They also want to put in a G-tube in. Jeff and I will be trained on how to feed via tube and how to keep it clean and everything.
- When we went back at 7:30 pm and he was crying so loud. It was a “gurgle” cry because of the secretions but he was screaming. I picked him up and he calmed down but it took several minutes of bouncing, whispering to him and rubbing his back.
Tuesday 9/22/09
- He was crying again when I got there with my mother. She heard him making his noises. I picked him up again and he stopped crying.
- They stopped the Reglan and bumped his feeds up to 45ml over 3 hours.
- PT came by and dropped off several exercises for me to do when I am sitting there. He is becoming a lot more limber and allowing me to work his legs and arms. There is some stiffness in his legs but they are becoming loose when I start working with him.
- Going to have a meeting with Geneticist on Thursday about genetic testing that has been done.
- 7lbs 11oz
- Took blood for the WCB storage or lysosomal enzyme test and sent it to Geneticist in Philadelphia.
Wednesday 9/23/09
- Today he had his hearing screened. She came at a bad time when he was eating. There was too much electric interference in the room and it was messing up the hearing machine and his feeding machine. She will come back at 8am when he is not eating and see what she can get from him. They can try up to 5 times when they are in the NICU.
- Up to 50ml over 3 hours and still off the Reglan.
- He was fussy today again. I love when he is making noises and wiggling.
- He has been keeping his saturation levels in the 90’s and when he is on my chest he can sat at 99 or 100 almost always. Something about my chest keeps his levels high.
- Upper GI is scheduled for Friday. I will find out the time on Thursday when they do their rounds.
Thursday 9/24/09
- Don’t know the time of the GI for Friday but I will call in the AM to find out.
- Spoke with Geneticist today. She confirmed that they sent out the blood on Tuesday. She also confirmed that he does not have adrenal leukodystrophy and probably not any kind. She measured his head and length. He is growing and she was pleased to see that.
- He was crying again today. I picked him up and he quieted it down.
- Tried to test hearing in the AM and couldn’t so they came back in the afternoon with a diagnostic one and they still couldn’t. His breathing was unregulated and they couldn’t get a good reading. They will try another day. She did mention to nurse that he might need to be sedated to get it done, who knows!
Friday 9/25/09
- They upped his feeds to 55ml and back on Reglan.
- The upper GI showed no reflux. NICU Pediatrician is going to talk with the NICU team and decide what is the best route to go as far as long term feedings. I am thinking a G tube and no fundo surgery.
- The reason for the upper GI is to see if there is an obstructions or twists in his GI tract; non-stricture- narrowing… he has no obstructions. This will help later on if he learns to mouth feed there will be nothing that would cause food or formula to go into the lungs and aspirate.
- This is not a test to see why he is not swallowing.. This has nothing to do with that function.
- I asked Leah about a swallow study and she mentioned that is up to the SLP and if they think James would be a good candidate for that. Nurse mentioned to me that in order to be part of a swallow study the child usually needs to be actively sucking or trying to suck.
- James is going to be sent to an audiologist when he is released from the NICU.
- Physical Therapist saw him today and worked him out.
- At 10:51pm, he was placed on oxygen again and had ANOTHER x-ray to see about infection, it was clear. His saturations were low according to his night nurse.
- Note: I was searching the internet and came across Moebius Syndrome and it sounds like James.
Saturday 9/26/09
- James’ morning nurse was concerned that his NJ tube was lose because it was measuring at 53 instead of 48 (nose to purple tip). They called for an x-ray and they said it is in place and to continue feeds. (1pm)
- They wanted James to have continuous feeds, which mean 14ml an hour for 4 hours… I think that is the calculation.
- 4pm back on oxygen and off of food. His saturation levels kept dropping. The docs and nurse think that the NJ tube is in place but not far enough.
- A surgeon came in, Pediatric General Surgeon, to talk to us about a procedure they are going to do on Monday, a PH Probe, it will check for acid reflux over a 24 hour period. They will look over those results, speak with us on Wednesday and he could have his G-tube in place on Friday.
- When we came back at 7 pm, he was off oxygen, the NJ and NG tubes were pulled and Robin was about to try to place the NJ tube again. The process started around 8 pm and we didn’t know if it was in place correctly until 11:30 pm. He had 2 more x-rays!
- He is back on his continuous feeds and will hopefully stay oxygen free.
Sunday 9/27/09
- He is eating 60ml over 3 hours every 9, 5, & 1 again.
- He had a great day today! :0)
Monday 9/28/09
- GI doctor came to speak with me about the PH Probe. He has to be off the Regland and Pepcid in order to place it. Hopefully it will be placed on Wednesday.
Tuesday 9/30/09
- The audiologist called to set up an appointment with me for Monday the 5th @ 2 pm to test him while he is sleeping on my chest.
- He is also going to be looked over by an orthopedic doctor to look at his spine.
- He is eating 75ml over an hour!
Wednesday 9/30/09
- Probe was not placed today. They will place it at the bedside sometime after 11 am. They will look over the results and set up a meeting early next week.
- Orthopedic doctor came to see him when I stepped out. I will call him and get report on Thursday
Thursday 10/1/09
- Probe placed at noon and will be taken out at noon Friday. They will love over results by the end of the day and hopefully have a family meeting on Monday and surgery on Wednesday.
- Orthopedic doctor got a hold of me and went over his observations. He said that James has hemivertebra (T10) also known as congenital scoliosis. He said there is nothing to worry about right now and to have another x-ray sometime between 6-12 months.
- Geneticist came to talk to me about the tests that another Geneticist wanted to run on James. She didn’t inform me on what they were called; she said if something comes up we will inform you otherwise don’t need to worry yourself. They are DNA tests that would be good info for other pregnancies.
Friday 10/2/09
- James was sating in the low 60’s for about ½ hour. He had about 3 spells that they had to use a bit of air flow to wake him back up. He was not taking enough big breaths.
- They took the tube out of his nose; he let out a big sneeze and then began sating back up into the 90’s. I am not sure if there was a correlation between the 2.
- Nurse thinks they will find something refluxing back up but another nurse does not think so. We will just have to wait until Monday to find out. The test was not read on Friday
- PT and SLP saw him today back to back and he was pooped!!
Saturday 10/3/09
- NICU Pediatrician said we should have a meeting Tuesday of next week hopefully surgery shortly after that. He was also telling us that there is no rush on having this surgery that is why it takes time.
- Back on his Pepcid and Regland.
- Nurse feels that an ENT should look at James and that there are things that can help his secretions. There is medicine that can help, or putting in a trach tube to release the fluids. She will mention it to morning nurse when she sees her in the morning and I will mention it as well.
Sunday 10/4/09
- The PH Probe was not read yet. Hopefully it will be read on Monday and we can schedule our meeting later this week.
Monday 10/5/09
- He is up to 80ml
- The ENT came to see James today. He fished a scope down his nose and looked at his nose and throat. He listened at his chest and heard some congestion. Everything structurally is good. Dr. was concerned that James did not cry during the procedure. That has something to do with this neurological impairments and him not being to feel discomfort or pain.
- The blood tests were drawn up today by nurse; the microarray test and the DNA test ( Alcardi-goutieres) genetic testing.
- PH Probe results came back and he has 11% reflux. Average or normal is between 5-7%.
Tuesday 10/6/09
- He is up to 85ml
- He turned his head when I came in to see him earlier. Mom was on one side of the crib and I was on the other and said “hello buddy”.
- Family meeting Wednesday 10/7/09 @ 1 pm with genetics, surgeon, and GI.
- He was awake for most of the day, eyes open and mouth closed.
Wednesday 10/7/09
- Family meeting today:
- She spoke to us about placing a g-tube into his belly along with a fundoplication. This would be a one time surgery and is not reversible. The fundoplication grows with him and will allow him to eat by mouth if he ever does. It will keep the acid from coming up and possibly burning his esophagus and cause more damage. After surgery he will be on a ventilator and pain meds for a few days. They will begin feeding him probably a day or so afterwards.
- This is a big decision and we can make it now or wait a week but I think we are leaning towards during this surgery Friday.
Thursday 10/8/09
- Stopped Reglan & Pepcid
Friday 10/9/09
- He had his surgery today. It was scheduled for 11:45 am but he didn’t go down until 1:45 pm and they said it was a 2 hour surgery but he didn’t get back upstairs until 5 pm!
- Pediatric General Surgeon said everything went great! They can start to use the tube probably Sunday or Monday.
- He also had his hearing checked when he came back because he was “under” and it didn’t really work. They got a preliminary test done and it shows that there is a loss but the more intense test that can show how much loss, he was moving. They said they would try again but we might just have to get him tested when he leaves the hospital.
- I called nurse at night and she said that he is doing great. He has calmed down and finally fell asleep. He will be on morphine for 48 hours and on a ventilator for 24 hours.
Saturday 10/10/09
- We got there around 3:30 pm to find him with nothing on at all!! No more tubes or ventilator!! He is still using his PICC line for fluids.
- His circumcision looks good. We just have to keep ointment on it when we change his diaper. We are hoping that it just heals while he is in the hospital and we don’t have to deal with it at home.
- He got his bed back when we went back at night. Nurse got him all settled in and I got to hold him in my arms while she was setting up his bed. He is getting to be a heavy one! My arm was starting to fall asleep a little bit.
Sunday 10/11/09
- The resident called us this morning around 10 am to tell us that they are going to start to use his g-tube to feed him Pedialyte. If everything goes in smooth they will start milk later today or Monday.
- He has taken 20-30ml of Pedialyte and for his 35ml he will be on breast milk…Woo Hoo!! They will increase by 5 with every feeding (every 4 hours) until he reaches 85ml.
Monday 10/12/09
- He should be at full feeds by 5 pm Tuesday!
- IV lipids and vitamins are done; he is on clear fluids, hyperol for a day or so. Once liquids are done he can get his PICC line out.
- They are going to try Robinul to decrease secretions later this week. His secretions are a lot less!
- Lysomal Enzyme were NORMAL!
Tuesday 10/13/09
- I got to the NICU and nurse was telling me that she had to give him a ½ a dose of morphine because he was very tense. He loosened up after that.
- Physical Therapists came by to work him. We worked on his neck and shoulders. After she was finished she wanted us to put him on his left side.
- I left James around 3:15 for break… around 4:30 I went to change him and I noticed his pillow was wet. I just assumed that he urinated on his bed but when I was changing him I noticed he had milk coming out of his g-tube site. We called the surgeon to come down. I waited until 5:15 and then left. When we came back around 7:45 the surgeon still didn’t arrive and James has not eaten since 1 pm. I was looking at his g-tube site and there was some old blood. I spoke with his nurse and she called the doc again to look at it. The surgical residents came and said the g-tube looks good and just decrease feeds. He is on 20ml overnight and we will see what happens in the morning. We need his g-tube to heal before we put to much milk on his belly.
Wednesday 10/14/09
- We received a phone call at 2:30 am (NICU Pediatrician) that they think James had seizures. He was given an EEG and seizure meds, which knocked him out. The doctors say that he will spring back once his body is use to the meds. He was given Ativan at 2:30 am and then Phenobarbital, every 12 hours.
- I will hopefully speak to Neurologist Thursday about what she saw and why didn’t any of the other EEG’s show seizures. I did speak with Dad’s cousin and he told me that it is a snap shot of his brain at that time and he might have been having these all along but we just didn’t catch them before. The meds will help him he said and this is the least of the worries with this kiddo.
Thursday 10/15/09
- Neurologist came by to speak with me about what she saw on the EEG from Wednesday morning. She said that she is 95% sure it was a seizure because of his movements and how the Ativan helped instantly. I did ask her a few questions:
- How long would he be on the Phenobarbital? As along as we think he needs to be. He will come in for a check up in a few months and we will check his levels and give him another EEG.
- Side effects of medication? Drowsy and maybe slow learning as he gets older.
- He had a spell last night with nurse. He dipped down into the 60’s and she couldn’t get him out of hit with gentle shaking and repositioning. She also wrote that she suctioned him and it was not working. They gave him Ativan thinking it was a seizure but that didn’t work so she bagged him. He had to be on oxygen form 5 am till 10 am. He was gasping for breath, they were thinking it was an obstruction in his throat from secretions.
Friday 10/16/09
- Off Oxygen as of 10 am
- Eating 80-90ml of milk over 2 hours, he seems to be handling it with no leakage. Pediatric General Surgeon came by to look at his g-tube and she said it looks great.
- Spoke with Social Worker about getting the ball rolling as far as setting up home health care and discharging him. We will have to do “care by parent” for a night or two before he comes home.
- ENT came by and looked him over. He has some fluid in his ears, I was not sure of what we are going to do about that. I asked and didn’t really get a straight answer. He is too young for tubes in his ears but it could have something to do with why he didn’t pass his hearing exams. He also said that James needs to be spell free for a few weeks before we can safely send him home. If he keeps having spells, we will have to discuss a trach or medication, but the medication might dry up the secretions but it might also dry him out. Not sure if we want to try that just yet.
Saturday 10/17/09
- He is on his maintenance dose of Phenobarbital and will be given this medication at 9 am and 9 pm at night via g-tube.
Sunday 10/18/09
- He is starting a smaller dose of Robinul to dry out the secretions…1.5ml every 8 hours.
- Still on 90ml over 2 hours.
Wednesday 10/21/09
- 100ml over 2 hours; his weight should have given him 110 but we decided on 100.
- Note: no Ferrell bag was used today.
- Home health came by to inform me that we will be getting our equipment on Monday to get trained on. She will show me how to use his feeding pump on Friday.
Thursday 10/22/09
- 110ml over 2 hours
- 2 leaks today. He was laying on me while eating and it leaked. There is nothing to be concerned about because the tube is still in place.
- Great SLP and PT sessions today!!!
Friday 10/23/09
- PICC line was taken out.
Wednesday 10/28/09
- G-tube sprung a leak, Pediatric General Surgeon put in his button.
- EEG again so see how his brain looks before heading home Thursday. She saw some spikes and upped his dose a little. He is taking 2.6 now.
Thursday 10/29/09
- He came home!!
- Phenobarbital: 20MG/5ML
- Robinul: .1MG/ML

Final Thoughts
The nurses in the NICU were fantastic. Many of his regular nurses follow him on Facebook to keep up to date on how he’s doing. That’s how much they care about their patients.
If you didn’t read all of the notes above, which I’m sure most of you didn’t, one thing we had to do prior to being discharged from the NICU was to do what they call “Care by Parent”. This is where you spend 1 or 2 nights in more of a private room within the NICU with your child. It’s kind of setup like a bedroom at home and includes any equipment you would have at home to care for your child. This experience gives the parents an opportunity to care for the child overnight without nurses, but also have nurses available for any questions or problems. Stacy was with James pretty much every day so she knew everything that was involved with taking care of James, but I found it helpful. After two months, I was ready to get my family home, but I was nervous at the same time. In the NICU, James was cared for around-the-clock by nurses, and now Stacy and I were going to be his sole caregivers. “Hope we don’t screw this up!” The “Care by Parent” helped ease some of that nervousness and show that we got this. At least we think we do. Bringing a “normal” baby home for the first time is an adjustment, but bringing a baby home with medical challenges is going to be an even bigger adjustment. By the time we finally got to take him home on October 29th, 2009, this is what we knew about James:
- He had an in utero stroke during the 1st trimester of pregnancy.
- He has no suck/swallow reflex so he was unable to take breast milk or formula from a bottle or clear his own secretions from his nose or throat.
- They originally inserted a feeding tube through his nose to his stomach as a way to feed him. He later had a surgery to insert a g-tube directly into his stomach.
- Because he was unable to clear his own secretions, James required frequent suctioning to clear his airways.
- James has Factor V Leiden blood clotting disorder.
- The optic nerve in his left eye never fully developed so he has vision issues.
- He doesn’t blink.
- He has a chromosome disorder called 22q11.2 duplication which means he has an extra copy of a small piece of chromosome 22.
- He had reflux and had Fundoplication surgery while in the NICU to prevent this reflux.
- He has quadriplegic cerebral palsy, which affects all 4 limbs.
- He has scoliosis, which is a sideways curvature of the spine.
- He has a seizure disorder.
Side note: I never understood why people say, “we’re pregnant”, when a couple is expecting a baby. “We” are not pregnant, only the woman is. Last time I checked, men can’t get pregnant, unless they’re Arnold Schwarzenegger in “Junior”. The man fertilizes the woman’s egg and SHE gets pregnant. She goes through all of the hormonal changes, the mood swings, the aches, the pains, the weird cravings. As the man, we don’t go through all of that. We might get random requests to stop on the way home from work to pick her up pickles and ice cream; or comfort her when she starts crying about something she normally wouldn’t cry over. The closest we can get to being pregnant, is the sympathy weight we gain while our wife or girlfriend is pregnant, but “we” are most definitely not pregnant.
After our heartbreaking experience with losing Jackson we quickly realized that sometimes life throws you unexpected curves. (Our tragic loss of Jackson was discussed in the Our Story.) When we…sorry, I mean when Stacy became pregnant with baby #2, we were happy, scared, and nervous all at the same time. By no means were we trying to replace Jackson. He will always be considered our first child, even though we never got the chance to meet or hold him. As a matter of fact, we sometimes refer to him as James’ big brother. We were a little surprised that Stacy got pregnant again so soon after losing Jackson. The sadness, emptiness, numbness, and anger were still so fresh when baby #2 came into the picture. Of course we were happy that we had a second chance to have a child, but we were understandably scared to death. “Would this child be “normal”?” We were a little bit stressed out waiting for all of the prenatal tests and ultrasounds to come back with the “all clear”. After everything we went through during our previous pregnancy, and ultimately losing Jackson, we decided to wait until our new baby appeared to be healthy before we told family and friends. Stacy was about 4 months along before we told anybody. Four months of waiting, nail biting, pacing, wondering, praying.

Needless to say, it was a very long four months. Once we received the final confirmation that this baby seemed healthy and normal, you could hear our sighs of relief. We continued with the routine OBGYN visits and ultrasounds, and everything seemed normal throughout the pregnancy. Then, on the night of August 28th, 2009, everything was about to change.
In the middle of dinner, Stacy’s water broke, and she immediately ran to the bathroom. As she was cleaning up, she noticed what appeared to be meconium in the amniotic fluid. Meconium, a newborn baby’s first poop, is made up of cells, fats, and intestinal secretions, and is usually passed in the first few hours or days after birth. When meconium is passed prior to birth, it can make it harder for the baby to breathe because it can clog the airways, irritate the airways and injure the lung tissue, and block surfactant, which is a fatty substance that helps open the lungs after birth. (The preceding information about meconium was taken from https://kidshealth.org/en/parents/meconium.html.)
We rushed to the hospital as fast as we could, but it still took us about 30 minutes. As we walked through the parking lot towards the ER, Stacy had a towel between her legs to absorb the amniotic fluid. We passed a woman in the parking lot who told us “congratulations”. Apparently, a woman waddling towards the hospital with a towel between her lets is a sign that she is about to have a baby.
Once we got settled into a room in Labor and Delivery, the nurses started the routine pre-delivery prep work. There was some concern that James wasn’t moving. One of the nurses reached up inside of Stacy to try to attach some probes to detect a heartbeat. When she lightly scratched his head and he still didn’t move, she feared that he was in distress and called for an emergency C-section. I can’t explain what we were feeling at that moment. We were in utter disbelief. How did we go from the Jackson pregnancy where we knew something was wrong early on, to this pregnancy where everything seemed normal, only to be thrown this curveball? “Was James okay?” “Please be okay!” “God, please don’t do this!”
When our OBGYN on-call arrived, Stacy was wheeled into delivery to get James out as quickly as possible. At 12:30 am on August 29th, James was brought into the world. I had seen enough movies and hospital shows to know that a baby cries shortly after it is born. But James didn’t cry. As we held our breathes waiting for him to cry, we were told that he was alive, but they weren’t sure what was wrong, so they were going to take him to the NICU for further observation and testing. The NICU, or Neonatal Intensive Care Unit, is similar to an Intensive Care Unit (ICU) for adults, but the NICU is for babies. Babies that are born premature, who have had a difficult birth, or who have health problems are sent to the NICU. There they receive around the clock care by a team of nurses, doctors, and specialists. We were fortunate enough that James was born in a hospital with one of the best NICUs in the area. If you want to read more about what a NICU is, please visit this page: https://kidshealth.org/en/parents/nicu-caring.html.
James ended up spending the first 2 months of his life in the NICU. During those long, emotional, and draining two months, he was poked, prodded, scanned, and assessed by several doctors and specialists trying to figure out what was wrong with him. By the time we finally got to take him home on October 29th, 2009, this is what we knew:
- James had an in utero stroke during the 1st trimester of pregnancy.
- He had no suck/swallow reflex so he was unable to take breast milk or formula from a bottle or clear his own secretions from his nose or throat.
- They originally inserted a feeding tube through his nose to his stomach as a way to feed him. He later had a surgery to insert a g-tube directly into his stomach.
- Because he was unable to clear his own secretions, James required frequent suctioning to clear his airways.
- James has Factor V Leiden blood clotting disorder.
- The optic nerve in his left eye never fully developed so he has vision issues.
- He doesn’t blink.
- He has a chromosome disorder called 22q11.2 duplication which means he has an extra copy of a small piece of chromosome 22.
- He had reflux and had Fundoplication surgery while in the NICU to prevent this reflux.
- He has quadriplegic cerebral palsy, which affects all 4 limbs.
- He has scoliosis, which is a sideways curvature of the spine.
- He has a seizure disorder
For further details about our two month stay in the NICU, please read the “Life in the NICU” post.
While the “What to Expect…” books are excellent, they did not prepare us for either one of our pregnancies. I don’t think anything could have prepared us for everything we went through. The one thing that got us through it all was each other. There were times when Stacy would break down and I would be the strong one. There were times when I would break down and Stacy had to be the strong one. And then there were times when we both just broke down, when all we could do was just hold each other. “What doesn’t kill you makes you stronger”. I think going through all of this has made Stacy and I a stronger, both as couple, and as individuals.
]]>