Disclaimer: The author of the content below is not a medical professional and does not have any medical training. As such, the contents on this page, including text, graphics, images, and any other material are for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Our full medical disclaimer can be found by clicking here.
If you’ve read Our Story, or some of the other posts on this site, you know that James had a stroke before he was born which we believe was the root cause to his many other medical issues. One of those issues is a seizure disorder.
During his two-month stay in the NICU after he was born, James exhibited what was thought to be a seizure. After we talked with a neurologist to discuss a plan of action, medications to treat the seizures, and what this meant going forward, we took to the Internet to find out more information.
Epilepsy is a big topic and I couldn’t possibly write about it all so I will just focus on answering the most common questions about seizures and epilepsy. This is not meant to be a “this is all you need to know about epilepsy” post. I have included links to the sites that I have referenced in this article that you can use to find more information. At the very bottom of this post, I have included a complete list of all the sites I have referenced throughout this article as well as some other sites that have good information about epilepsy and seizures. If you are looking for further information regarding epilepsy or seizures, please refer to those sites, and consult with your doctor or other healthcare professional.
Since this is an extremely long post, to make it easier to navigate I have made the following list of questions clickable. If there is a particular question you are curious about, click on it to be taken directly to the answer to that question. Then you can simply hit the back button in your browser to be brought back to the list of questions. Or, if you prefer, you can just read (or skim) this entire article from top to bottom. The choice is yours. But be warned…this is a very long read!
If someone has a seizure, do they have epilepsy?
Are there different types of seizures?
What is the difference between epilepsy and seizures?
What are the signs or symptoms of a seizure?
Can someone die from epilepsy?
What is Sudden Unexpected Death in Epilepsy (SUDEP)?
Can someone with epilepsy exercise and/or play sports?
Do people who have epilepsy also have developmental disabilities?
What should I do if I see someone having a seizure?
Where can I find more information about epilepsy and seizures?
What is a seizure?
Mayo Clinic defines seizure as “a sudden, uncontrolled electrical disturbance in the brain. It can cause changes in your behavior, movements or feelings, and in levels of consciousness. If you have two or more seizures or a tendency to have recurrent seizures, you have epilepsy.”
Healthline says that seizures are “changes in the brain’s electrical activity. These changes can cause dramatic, noticeable symptoms, or in other cases no symptoms at all. The symptoms of a severe seizure include violent shaking and a loss of control. However, mild seizures can also be a sign of a significant medical problem, so recognizing them is important. Because some seizures can lead to injury or be a sign of an underlying medical condition, it’s important to seek treatment if you experience them.”
What is epilepsy?
Epilepsy Ontario describes epilepsy as “a common brain (neurological) disease characterised by recurrent seizures, which are brief disruptions in normal brain activity that interferes with brain function. Seizures can manifest as full-body convulsions, but there are many kinds – with some types, you might not even notice a seizure at all. Currently there is no cure, and for many it is lifelong.”
WebMD says pretty much the same thing, but with some different terminology. “Epilepsy is a chronic (long-lasting) medical condition marked by recurrent epileptic seizures. An epileptic seizure is an event of altered brain function caused by abnormal or excessive electrical discharges from brain cells. Epilepsy is one of the most common neurologic disorders, affecting up to 1% of the U.S. population.”
If someone has a seizure, do they have epilepsy?
You may have noticed in the answer to the previous question that both WebMD and Epilepsy Ontario mentioned “recurrent seizures”. If someone has a single seizure, they don’t necessarily have epilepsy. A person is only diagnosed as having epilepsy after they have experience two or more seizures. Although James was thought to have had a seizure in the NICU, he wasn’t diagnosed with epilepsy until much later…after he had additional seizures, and some additional testing was performed. Diagnosing epilepsy will be discussed in more detail below, under “how is epilepsy diagnosed”.
How long do seizures last?
The length of a seizure can vary depending on what type of seizure it is. Most seizures last from 30 seconds to a couple of minutes. Any seizure that lasts longer than 5 minutes is considered a medical emergency. Seek medical attention immediately.
Are there different types of seizures?
In 1981 the International League Against Epilepsy (ILAE), the world’s main scientific body devoted to the study of epilepsy, developed an international classification of epileptic seizures that divided seizures into two major classes: partial-onset seizures and generalized-onset seizures.
In 2017 the ILAE revised its classification of seizures to make diagnosing and classifying seizures easier and more accurate by incorporating three key features:
- Where the seizure(s) began in the brain.
- The level of awareness during the seizure(s).
- Other features of the seizure(s).
As you can see in ILAE’s 2017 classification chart below, most seizures can be categorized as either focal onset or generalized onset depending on where in the brain they occur and how they began. In some cases, however, it is unknown where and how the seizure began. These are referred to as unknown onset seizures.
Note that partial-onset seizures in the 1981 classification were renamed focal onset seizures in the 2017 revision. You may see or hear both of these terms used interchangeably.
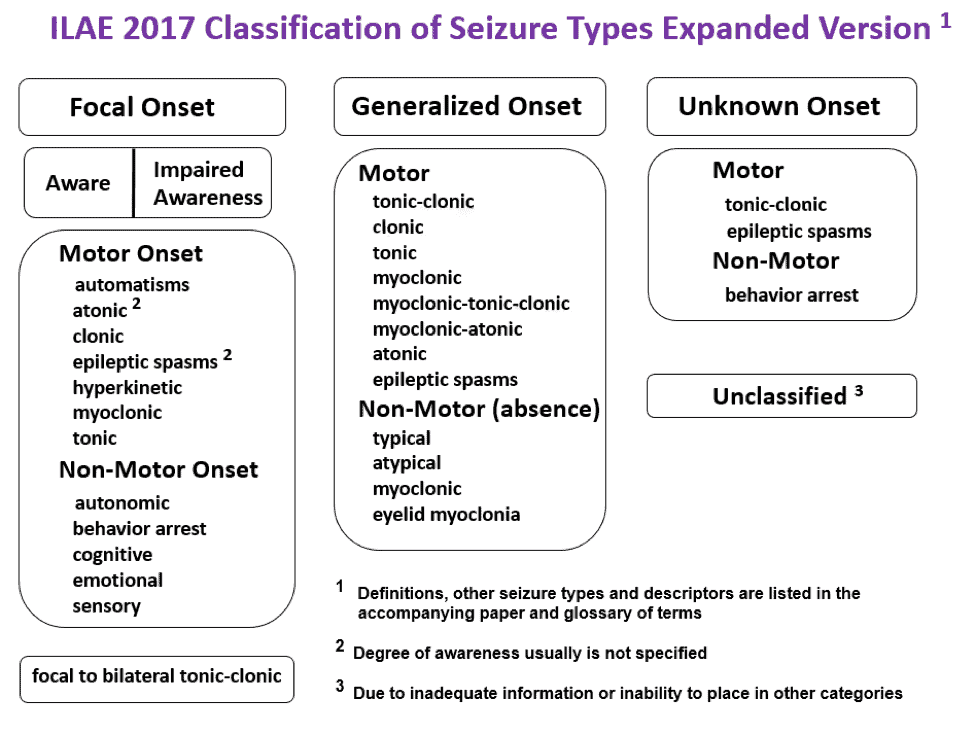
If you’re like me the first time I saw this chart, you are probably feeling a bit overwhelmed. While there is a lot of stuff on the chart, I’ll try to break it down for you.
As I mentioned above, seizures fall under three (3) main categories: focal, generalized, and unknown.
Focal onset seizures occur in one area of the brain. Prior to ILAE’s 2017 classification revision, focal onset seizures were referred to as partial onset seizures. Focal onset seizures can be further categorized as either focal aware or focal impaired awareness.
- In focal aware seizures (also referred to as focal onset aware seizures, simple focal seizures, or focal seizures without loss of consciousness), a person remains conscious and is aware of their surroundings. During this type of seizure, a person may experience an involuntary jerking of a body part such as an arm or leg. Prior to the 2017 revision, focal aware seizures were called simple partial seizures.
- During a focal impaired awareness seizure (or complex focal seizure or focal onset impaired awareness seizure) a person may lose consciousness and is unaware that the seizure is happening. Before the 2017 revision, focal impaired awareness seizures were called complex partial seizures.
- In some cases it is hard to determine if a person is aware or is impaired during a seizure. In situations like these, we can look at the motor symptoms that the person may be experiencing.
-
-
- The ILAE says that “a motor onset seizure involves motor activity (movement) and may be due to either an increase or decrease in contraction in a muscle or group of muscles.” I have listed the types of motor onset seizures below along with a brief description of each. I have included links to International League Against Epilepsy webpages if you would like further information about a specific type of seizure listed below. Links will open in new browser tabs.
-
-
-
-
-
- Automatisms: a coordinated, repetitive motor activity, often resembling a voluntary movement, but undertaken without volition.
-
-
-
-
-
-
-
- Atonic: sudden loss or diminution of muscle tone without apparent preceding myoclonic or tonic activity, typically lasting >500 milliseconds but < 2 seconds. It may involve the head, trunk, jaw or limb musculature.
-
-
-
-
-
-
-
- Clonic: the movement involves sustained rhythmic jerking, this may involve a distal limb, one limb or one side of the body. The jerking may spread to involve parts of the body according to their representation on the motor cortex (according to the homunculus), this is known as a Jacksonian march.
-
-
-
-
-
-
-
- Epileptic spasms: a sudden flexion, extension or mixed flexion-extension of proximal and truncal muscles, lasting 1-2 seconds i.e. longer than a myoclonic jerk (which lasts milliseconds) but not as long as a tonic seizure (which lasts > 2 seconds).
-
-
-
-
-
-
-
- Hyperkinetic: involves movements of proximal limb or axial muscles, producing irregular large amplitude movements, such as pedaling, pelvic thrusting, jumping, thrashing and/or rocking movements.
-
-
-
-
-
-
-
- Myoclonic: a single or short cluster of brief muscle contractions (jerks), each jerk is typically milliseconds in duration.
-
-
-
-
-
-
-
- Tonic: increased muscle tone, usually lasting for seconds to minutes.
-
-
-
-
-
- Epilepsy Action describes focal non-motor onset seizures as seizures “where the main symptoms don’t involve muscle activity. They can include things like changes in emotions, thinking and sensations.” The types of non-motor onset seizures are listed below with a brief description of each. I have included links to International League Against Epilepsy webpages if you would like further information about a specific type of seizure listed below. Links will open in new browser tabs.
-
-
-
-
-
- Autonomic: affects the part of the brain responsible for involuntary functions. These seizures may cause changes in blood pressure, heart rhythm, or bowel or bladder function.
-
-
-
-
-
-
-
- Behavior arrest: characterized by a decrease in amplitude and/or rate or arrest of ongoing motor activity during the seizure. Because brief behaviour arrest is common and difficult to identify at the start of many seizures, the arrest must be persistent and dominant through the entire seizure.
-
-
-
-
-
-
-
- Cognitive: involves an alteration in a cognitive function (which can be a deficit or a positive phenomenon such as forced thought), which occurs at seizure onset. To be classified as a focal cognitive seizure, the change in cognitive function should be specific and out of proportion to other relatively unimpaired aspects of cognition, because all cognition is impaired in a focal impaired awareness seizure.
-
-
-
-
-
-
-
- Emotional: characterized by alterations in mood or emotion, or the appearance of altered emotion without the subjective emotion, at seizure onset.
-
-
-
-
-
-
-
- Sensory: affecting the senses, such as: hearing problems, hallucinations and olfactory or other distortions.
-
-
-
Whereas focal onset seizures start in a single part of the brain, generalized onset seizures affect both sides of the brain at the same time. If you notice in ILAE’s chart above, the generalized onset column does not include aware and impaired awareness like focal onset did. Instead, it jumps right into Motor onset and non-motor (absence) onset.
Let’s take a look at each type of seizure that falls under generalized onset. Just like I did above with focal onset seizures, I will include a brief description of each specific seizure and include links to International League Against Epilepsy webpages if you would like further information about these seizures. These links will open in new browser tabs.
- Motor Onset Generalized Seizures
-
-
- Atonic: involves sudden loss or diminution of muscle tone without apparent preceding myoclonic or tonic features. Atonic seizures are very brief (<2 seconds) and may involve the head, trunk or limbs. Atonic seizures often occur in individuals with intellectual impairment.
-
-
-
- Clonic: bilateral sustained rhythmic jerking
-
-
-
- Epileptic spasms: a sudden flexion, extension or mixed flexion-extension of proximal and truncal muscles, lasting 1-2 seconds i.e. longer than a myoclonic jerk (which lasts milliseconds) but not as long as a tonic seizure (which lasts > 2 seconds). Spasms typically occur in a series, usually on wakening. Subtle forms may occur with only chin movement, grimacing, or head nodding. Spasms may be bilaterally symmetric, asymmetric, or unilateral, depending on whether they are generalised onset or focal onset.
-
-
-
- Myoclonic: a single or series of jerks (brief muscle contractions). Each jerk is typically milliseconds in duration. Myoclonic status epilepticus is characterized by ongoing (> 30 minutes) irregular jerking, often with partially retained awareness. These two features distinguish a myoclonic status epilepticus from a generalized clonic seizure (see above), where consciousness is lost and the jerking is sustained and rhythmic.
-
-
-
- Myoclonic-atonic: a myoclonic seizure followed by an atonic seizure. Sometimes a series of myoclonic jerks occurs prior to the atonia. The head and limbs are affected, typically resulting in rapid fall. The myoclonic jerk may be subtle.
-
-
-
- Myoclonic-tonic-clonic: see tonic-clonic (and variants) below.
-
-
-
- Tonic: involves bilaterally increased tone of the limbs typically lasting seconds to a minute. They often occur out of sleep and in runs of varying intensity of tonic stiffening. The individual is unaware during these events. At the beginning of tonic seizures with more intense stiffening, individuals may make an expiratory sound. More severe and prolonged tonic seizures may have a vibratory component which may be confused with clonic jerking. Tonic seizures often occur in individuals with intellectual impairment.
-
-
-
- Tonic-clonic (and variants): bilateral and symmetric generalized motor seizures, that occur in an individual with loss of consciousness. The tonic-clonic seizure consists of a tonic (bilateral increased tone, lasting seconds to minutes) and then a clonic (bilateral sustained rhythmic jerking) phase, typically in this order, however variations such as clonic-tonic-clonic and myoclonic-tonic-clonic can also occur.
-
- Non-Motor (absence) Generalized Seizures
-
-
- Atypical – less abrupt onset and offset of loss of awareness than typical absence seizures. They are often associated with other features such as loss of muscle tone of the head, trunk or limbs (often a gradual slump) and subtle myoclonic jerks. Atypical absence seizures often occur in individuals with intellectual impairment. The loss of awareness may be minimal with the patient continuing an activity, but more slowly or with mistakes.
-
-
-
- Eyelid myoclonia – absence seizure accompanied by brief, repetitive, often rhythmic, fast (4-6 Hz) myoclonic jerks of the eyelids with simultaneous upward deviation of the eyeballs and extension of the head. Seizures are typically very brief (<6s in duration) and multiple seizures occur on a daily basis. Mostly awareness is retained.
-
-
-
- Myoclonic – rhythmic myoclonic jerks of the shoulders and arms with tonic abduction that results in progressive lifting of the arms during the seizure. The myoclonic jerks are typically bilateral but may be unilateral or asymmetric. Perioral myoclonias and rhythmic jerks of the head and legs may occur. Seizures last 10-60 seconds and typically occur daily. Level of awareness varies from complete loss of awareness to retained awareness.
-
-
-
- Typical – a generalized seizure with abrupt onset and offset of altered awareness which can vary in severity (see specific syndromes). Memory for events during the seizures is usually impaired although there may be some retained awareness particularly for adolescents. Clonic movements of eyelids, head, eyebrows, chin, perioral or other facial parts may occur, most typically at 3Hz. Myoclonus of limbs can rarely occur. Oral and manual automatisms are common and there may be perseveration of behaviors occurring prior to seizure onset.
-
Unknown Onset Seizures
By now you should have a basic understanding of focal onset and generalized onset seizures. Part of the process of classifying a seizure as either focal or generalized relies on visual cues. What was the person doing when the seizure started? What sort of movements were they making? Did they appear to be alert and aware or did they seem impaired?
But what if nobody is there to see a person having a seizure? As the Epilepsy Foundation explains, “when the beginning of a seizure is not known, it’s now called an unknown onset seizure. A seizure could also be called an unknown onset if it’s not witnessed or seen by anyone, for example when seizures happen at night or in a person who lives alone. As more information is learned, an unknown onset seizure may later be diagnosed as a focal or generalized seizure.”
Just like the focal onset and generalized onset seizures, unknown onset seizures can be further classified as either motor or non-motor types.
- Motor Unknown Onset Seizures
-
- Epileptic spasms – a sudden flexion, extension or mixed flexion-extension of proximal and truncal muscles, lasting 1-2 seconds i.e. longer than a myoclonic jerk (which lasts milliseconds) but not as long as a tonic seizure (which lasts > 2 seconds). Spasms typically occur in a series, usually on wakening. Subtle forms may occur with only chin movement, grimacing, or head nodding. Spasms may be bilaterally symmetric, asymmetric, or unilateral, depending on whether they are generalised onset or focal onset.
-
-
-
- Tonic-clonic (and variants) – bilateral and symmetric generalized motor seizures, that occur in an individual with loss of consciousness. The tonic-clonic seizure consists of a tonic (bilateral increased tone, lasting seconds to minutes) and then a clonic (bilateral sustained rhythmic jerking) phase, typically in this order, however variations such as clonic-tonic-clonic and myoclonic-tonic-clonic can also occur.
-
- Non-Motor Unknown Onset Seizures
-
- Behavior arrest: characterized by a decrease in amplitude and/or rate or arrest of ongoing motor activity during the seizure. Because brief behaviour arrest is common and difficult to identify at the start of many seizures, the arrest must be persistent and dominant through the entire seizure.
-
What is the difference between epilepsy and seizures?
Simply put, a seizure is a single occurrence. Epilepsy, on the other hand, is a neurological condition characterized by two or more seizures. So a person who has a single seizure does not necessarily have epilepsy.
What are the signs or symptoms of a seizure?
Mayo Clinic lists the following signs and symptoms of a seizure:
- “Temporary confusion
- A staring spell
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
- Cognitive or emotional symptoms, such as fear, anxiety or déjà vu”
The Epilepsy Foundation has a much longer list:
- “Odd feelings, often indescribable
- Unusual smells, tastes, or feelings
- Unusual experiences – “out-of-body” sensations; feeling detached; body looks or feels different; situations or people look unexpectedly familiar or strange
- Feeling spacey, fuzzy, or confused
- Periods of forgetfulness or memory lapses
- Daydreaming episodes
- Jerking movements of an arm, leg, or body
- Falling
- Tingling, numbness, or feelings of electricity in part of the body
- Headaches
- Unexplained confusion, sleepiness, weakness
- Losing control of urine or stool unexpectedly”
What causes epilepsy?
CureEpilepsy.org says that “epilepsy and seizures result from abnormal circuit activity in the brain. Any event ranging from faulty wiring during brain development, brain inflammation, physical injury or infection can lead to seizure and epilepsy. However, according to recent estimates, in up to 50% of patients diagnosed with epilepsy, the cause is unknown (idiopathic).” They go on to list the following known causes of epilepsy:
- “Genetics
- Brain structure abnormalities
- Metabolism changes
- Immune system abnormalities
- Trauma
- Stroke
- Tumors
- Infectious disease”
If you’ve been following James’ story, you know that his epilepsy is more than likely caused by the stroke he suffered in utero.
Can epilepsy be prevented?
If you haven’t done so already, go back to the previous question and look over the known causes of epilepsy. In order to prevent epilepsy, we would need to eliminate those causes. While we can’t eliminate some of those causes, like genetics or immune system abnormalities, we can take precautions to prevent other causes like head trauma. The US Centers for Disease Control and Prevention lists the following measures we can take to prevent a traumatic brain injury:
- Ride safely. Use safety belts, child passenger seats, airbags, bicycle helmets, and motorcycle helmets to reduce motor vehicle and traffic injuries.
- Step carefully. Falls are the leading cause of brain injury. Older adults and children have an increased chance of brain injuries from falls.
- Get help for traumatic brain injuries if they happen. The chance of epilepsy is high with severe brain injuries. Taking good care of the injury may help to avoid epilepsy.
How common is epilepsy?
According to the Epilepsy Foundation:
- Seizures and epilepsy are more common in young children and older people.
- About 1 in 100 people in the U.S. has had a single unprovoked seizure or has been diagnosed with epilepsy.
- 1 in 26 people will develop epilepsy in their lifetime. People with certain conditions may be at greater risk.
- Each year, about 48 of every 100,000 people will develop epilepsy. However, seizures may occur more often in different age groups (very young and older people), in different races, and in different areas of the world.
- According to the August 11, 2017, “Morbidity and Mortality Weekly Report” from the Centers for Disease Control and Prevention (CDC), at least 3.4 million people in the U.S. live with seizures, including 470,000 children.
- Epilepsy is the 4th most common neurological condition and epilepsy affects more than 65 million people worldwide.
- More men than women have epilepsy overall by a small amount.”
How is epilepsy diagnosed?
Diagnosing epilepsy is not always easy. It’s not as simple as having a couple of tests done. Yes, there may be some testing done, but there is more to a diagnosis than that. A doctor will also want to know what happened before, during and after a seizure to help in the diagnosis. For this reason, it is important to make some notes about your seizure(s). If you have a seizure you may not know or remember what happened, so if there someone else there that witnessed it, have them make some notes for you.
The following list of questions, courtesy of Epilepsy Society, may help you or someone who witnessed your seizure make useful notes about what happened:
Before the seizure
-
- Did anything trigger (set off) the seizure – for example, did you feel tired, hungry, or unwell?
- Did you have any warning that the seizure was going to happen?
- Did your mood change – for example, were you excited, anxious or quiet?
- Did you make any sound, such as crying out or mumbling?
- Did you notice any unusual sensations, such as an odd smell or taste, or a rising feeling in your stomach?
- Where were you and what were you doing before the seizure?
During the seizure
-
- Did you appear to be ‘blank’ or stare into space?
- Did you lose consciousness or become confused?
- Did you do anything unusual such as mumble, wander about or fiddle with your clothing?
- Did your colour change (become pale or flushed) and if so, where (face or lips)?
- Did your breathing change (for example, become noisy or look difficult)?
- Did any part of your body move, jerk or twitch?
- Did you fall down, or go stiff or floppy?
- Did you wet yourself?
- Did you bite your tongue or cheek?
After the seizure
-
- How did you feel after the seizure – did you feel tired, worn out or need to sleep?
- How long was it before you were able to carry on as normal?
- Did you notice anything else?
Watching someone have a seizure is hard. You feel so helpless and don’t know what to do. You’re probably not thinking straight. But if you can, jot down some notes. Or if you have a cell phone, take a video that can be shown to a doctor. If you do witness someone having a seizure, there are a couple of safety precautions you should take before taking any notes or video of the event. Please refer to, ‘what should I do if I see someone having a seizure’ for some safety precautions you should take if you see someone having a seizure.
In addition to the answers to the above questions, a doctor will also want to review your medical history and other medical conditions as part of the diagnosis.
He or she may also want to run some tests which may include:
- Blood test
- CT (computerized tomography) scan which uses X-rays to obtain cross-sectional images of your brain which might reveal abnormalities that might be causing your seizures.
- EEG (electroencephalogram) to check for patterns of normal or abnormal brain electrical activity.
- MRI (magnetic resonance imaging) scan which uses powerful magnets and radio waves to create a detailed view of your brain which may show lesions or abnormalities that could be causing your seizures.
- PET (positron emission tomography) scan which uses a small amount of low-dose radioactive material that’s injected into a vein to help visualize active areas of the brain and detect abnormalities.
- SPECT (single-photon emission computerized tomography) test which uses a small amount of low-dose radioactive material that’s injected into a vein to create a detailed, 3D map of blood flow activity in your brain during seizures.
- Neuropsychological tests to assess your thinking, memory and speech skills. This test can help doctors determine which areas of your brain are affected.
How is epilepsy treated?
There are three (3) main treatments for epilepsy: medication, therapy, and surgery. Doctors will generally start with medication(s) and if that doesn’t work to improve or eliminate seizures, they may look at surgery or therapy.
Medication
James has been on several different medications to treat his seizures. As someone who suffers from bipolar depression, I was already aware that trying to find a medication to treat James’ epilepsy was going to be a bit hit-and-miss. The brain is a complicated thing. A medication that works for one person may not work as well (or at all) for another person.
If you are interested in what medications are currently available to treat seizures and epilepsy, please visit the Epilepsy Foundation’s Seizure Medication List site. There you can find in-depth information for the various medications including what the drug is used to treat, the forms they come in (tablet, liquid, IV), and dosing. They also answer commonly asked questions for many of the medications.
I also want to mention that sometimes a single medication doesn’t always work and a doctor or neurologist may prescribe more than one medication. James is currently (2020) taking two drugs to treat his epilepsy and they seem to be keeping his seizures under control. I also want to point out that it took us years to get to this point. Like I mentioned previously, it was a lot of trial and error to find the medications that would successfully treat his seizures. So try not to be too discouraged if the first few medications don’t work.
Therapy
The Mayo Clinic lists three (3) therapies that can be used in addition to, or in place of medication(s): vagus nerve stimulation, ketogenic diet, and deep brain stimulation.
- Vagus nerve stimulation (VNS)
James has one of these. A vagus nerve stimulator (VNS) is implanted underneath the skin of the chest. It has wires that attach to the vagus nerve in the neck. The VNS sends a pulse or a shock through the wires, into the vagus nerve, which then get sent into the brain.
By placing a special “wand” over the chest where the VNS is implanted, the doctor is able to program it, turn it on or off, and check statistics of the VNS like battery level, and how many times it has fired electrical signals to the brain.
Once programmed, the VNS is pretty much automatic and a sends a certain amount of millivolts to the brain at intervals that are pre-determined by the doctor. It also comes with a special magnet that can be used to manually trigger the VNS to send a jolt to the brain when a seizure is in progress to try and stop the seizure.
Because it is battery powered, it will need to be replaced every five (5) years or so, depending on the frequency of the pulses and the amount of current sent to the brain. James is currently on his 2nd one. He had the first one implanted in September of 2012, and the second one in March of 2017. Like I mentioned earlier, the doctor will be able to tell when it is due for replacement by using the magic “wand” and looking at the current battery level.
I also want to note that James uses the VNS in addition to medications.
- Ketogenic diet
You may have heard of the ketogenic diet (or keto diet) being used by adults for weight loss. The keto diet is a high-fat, low-carb diet that has also been shown to be effective in controlling seizures and infantile spasms.
Johns Hopkins All Children’s Hospital says that “children with seizures that are not well-controlled by medicines (called intractable epilepsy) and severe epilepsy syndromes (such as infantile spasms or Lennox-Gastaut syndrome) might benefit from a ketogenic diet.”
The Epilepsy Foundation also mentions that “the ketogenic diet has been reported to be safe, well tolerated and possibly effective for treating children with infantile spasms who do not respond to ACTH or steroid and vigabatrin.”
Infantile spasms, or IS, is a seizure disorder in babies. If you would like to find out more about infantile spasms, I wrote an article about it, which can be found here. Link will open in a new browser tab.
Although James did suffer from infantile spasms, we did not use the ketogenic diet to treat them because James’ IS were brought under control through the use of Vigabatrin (Sabril). We did, however, try to the keto diet about 6 months after James stopped taking Sabril to try to bring his seizures under control. He was on the keto diet for about 5 months and unfortunately it did not help with his seizures. He ended up losing a lot of weight to the point that he looked “sickly” as Stacy puts it. We took him off the keto diet and started trying different combinations of anti-seizure medications to try and bring his seizures under control.
As with other treatments, there are some risks and side effects with the ketogenic diet including constipation, dehydration, high cholesterol, kidney stones, slowed growth, and weak bones.
As I mentioned in the medications section above, not all children react the same way to treatments. Just because keto didn’t work for James doesn’t necessarily mean it will not work for your child.
- Deep Brain Stimulation (DBS)
Deep brain stimulation, or DBS, is similar to the VNS mentioned above in that it sends electrical impulses to the brain. Like the VNS, deep brain stimulation includes a device implanted in the chest. However, instead of attaching to the vagus nerve in the case of the VNS, the DBS uses electrodes that are implanted directly into the brain.
The Epilepsy Foundation explains two situations in which DBS may be used as a treatment option:
-
-
- “DBS may be used to treat people 18 years and older with uncontrolled focal seizures when medicines don’t work. Uncontrolled seizures, also called drug resistant seizures, are seizures that do not respond to appropriate trials of seizure medicines.
-
-
-
- DBS is an option for people whose seizures are not able to be treated with other types of epilepsy surgery.”
-
Deep brain stimulation is a relatively new treatment and was approved by the U.S. Food and Drug Administration (FDA) in 2018. Click the link to be redirected to the FDA website to find out more information about the Medtronic DBS system for epilepsy. Link will open in new tab.
Surgery
Like deep brain stimulation (DBS) mentioned above, epilepsy surgery might be an option for people who have seizures that don’t respond to medications or other therapies. There are several different types of surgery available; the type of surgery is dependent on the type of seizure a person has and where the seizures begin in the brain.
The Epilepsy Foundation has a wealth of information available for the different types of surgery so I won’t regurgitate that information here. I will simply list the types of surgeries and a brief synopsis of each. If you want further information on these surgeries, follow the link to the Epilepsy Foundation’s Epilepsy Surgery page. Link will open in new browser tab.
-
- Anatomical or Functional Hemispherectomy and Hemispherotomy: These types of epilepsy surgery are almost exclusively performed in children with seizures coming from a large area on one side of the brain (hemisphere). The procedures involve separating the area of seizure onset from the rest of the brain.
-
-
-
- Anatomical Hemispherectomy involves removing the frontal, parietal, temporal, and occipital lobes on one side of the brain. Deeper brain structures (basal ganglia and thalamus) are left in place. This type of hemisphere surgery has higher risk and is usually considered for people with hemimegalencephaly (a rare condition where one side of the brain is abnormally larger than the other).
-
-
-
-
-
- Functional Hemispherectomy involves removing a smaller area of the affected hemisphere and disconnecting the remaining brain tissue. This surgery involves less risk but is only helpful in a select group of people.
-
-
-
-
-
- Hemispherotomy is different than hemispherectomy as less brain tissue is removed to decrease the risk of complications from surgery. In this type of surgery, the surgeon makes a hole or several holes in the hemisphere instead of removing large sections of the brain.
-
-
-
- Corpus Callosotomy is usually reserved for people with severe generalized epilepsy (seizures involving both sides of the brain) who are subject to drop attacks (atonic seizures) and falls. The procedure involves splitting the main connection pathway between the two cerebral hemispheres (sides of the brain). Individuals being considered for this operation usually have:
-
-
-
- Frequent tonic, atonic, atypical absence, or tonic-clonic seizures
-
-
-
-
-
- Developmental delay
-
-
-
-
-
- Disabling seizure-related falls
-
-
-
- Focal Resection: this is the most common type of epilepsy surgery. It involves removing the area of the brain that is causing the seizures. Because it involves removing part of the brain, this type of surgery is reserved for people whose seizures start in non-critical parts of the brain. There are several types focal resection surgery:
-
-
-
- Temporal Lobe Resection: removes a portion of the temporal lobe of the brain. This type of surgery has the highest rate of success and is the most common type of epilepsy surgery.
-
-
-
-
-
- Frontal Lobe Resection: removes an area in the frontal lobe of the brain. This is the second most common type of epilepsy surgery.
-
-
-
-
-
- Parietal Lobe or Occipital Lobe Resection: removes a part or one of these lobes. This type of surgery is usually performed when an area in one of these lobes is found to contain abnormal structure or a lesion.
-
-
-
- Laser Interstitial Thermal Therapy (LITT): with the help of MRI to show the exact area of the brain to operate on, a laser is delivered with pinpoint accuracy to eliminate the seizure focus. This surgery is a minimally invasive procedure because there is no need to open the skull.
-
- Lesionectomy: removes a lesion that causes focal seizures.
-
- Multiple Subpial Transections (MSP): the neurosurgeon makes a series of fine shallow cuts (transections) in the brain’s gray matter. The cuts work by interrupting fibers that are thought to be involved in the spread of electrical seizure activity.
-
- Neurostimulation Device Implantations
-
-
-
- Deep Brain Stimulation (DBS) was briefly discussed above in the therapy section. The surgery to implant the device involves placing the device under the skin in the chest and implanting the electrodes into the brain. The device sends electrical impulses through the electrodes into the brain to stop the signals that trigger a seizure.
-
-
-
-
-
- Vagus Nerve Stimulation (VNS) was also discussed above in the therapy section. Similar to the DBS, surgery involves placing the device under the skin in the chest. Instead of implanting electrodes in the brain like the DBS, the VNS uses a wire that is attached to the vagus nerve in the neck. The VNS sends electrical impulses through the vegus nerve which then travel to the brain.
-
-
-
-
-
- Responsive Neuro Stimulation (RNS) is a device that is implanted in the skull with electrodes that are placed on or in the brain in the area where seizures begin. The RNS can record seizure activity directly from the brain, detect seizure onset, and then deliver an electrical stimulation to stop the seizure.
-
-
-
- Stereotactic Radiosurgery uses many precisely focused radiation beams to treat the area of the brain where seizures begin. The surgeon does not need to open the skull for the procedure so it is considered minimally invasive. The surgery uses 3D imaging to target high doses of radiation to the seizure focus with minimal impact on the surrounding healthy tissue.
Who treats epilepsy?
A neurologist is a doctor that specializes in diagnosing, treating and managing disorders of the brain and nervous system. These disorders include, but are not limited to, epilepsy, Alzheimer’s disease, multiple sclerosis, Parkinson’s disease, and stroke.
Pediatric neurologists are neurologists that specialize in diagnosing and treating neurologic disorders in children.
An epileptologist is a neurologist or pediatric neurologist who specializes in the treatment of epilepsy.
Neurosurgeons specialize in neurosurgery. Neurosurgery is surgery of the nervous system which includes the brain, spinal cord and spinal column, and peripheral nerves.
How can I/we manage epilepsy?
Although there are numerous medicines, therapies, and surgeries available to treat epilepsy, it should be noted that none of these are cures, and there is always a risk of having another seizure. There are, however, steps that you can take to help reduce the chances of having another seizure. The Managing Epilepsy Well Network provides a lot of useful information to help you manage your epilepsy. One of the tools that they offer is a self-management checklist. I have provided items on the checklist below. To view, download or print a PDF of the checklist, click here.
- Know about your condition.
- Take your seizure medicines as prescribed.
- Keep a record of your seizures and seizure triggers to track patterns and learn how to avoid seizure triggers.
- Check with your doctor before taking other medicines or supplements.
- Get help for emotional problems.
- Keep other health conditions in check.
- Get at least 7 to 8 hours of sleep each night.
- Have confidence to advocate for yourself.
- Talk to your doctor about health concerns.
- Practice ways to lower stress.
- Don’t use tobacco, drink alcohol excessively, or abuse other substances.
- Exercise regularly and safely each day.
- Follow a well-balanced diet and keep a healthy weight.
- Use memory strategies to help with memory problems.
- Keep in touch with friends and family for support.
Can someone die from epilepsy?
Most people with epilepsy live full and healthy lives, but unfortunately some people do die from epilepsy. The Epilepsy Foundation lists the following causes of death due to epilepsy:
- “Some people with epilepsy may lose their lives from accidents, suicide, or the underlying cause of their condition, such as brain tumors or infections.
- Another rare cause of epilepsy related death is New-onset refractory status epilepticus (NORSE), which is defined as refractory status epilepticus without an obvious cause after initial investigations.
- Yet, the leading cause of epilepsy-related death is believed to be sudden unexpected death in epilepsy, also known as SUDEP.”
If you would like to learn more about NORSE or SUDEP, please click on the links above to be redirected to the Epilepsy Foundation’s website.
What is Sudden Unexpected Death in Epilepsy (SUDEP)?
As the name says, SUDEP is the sudden, unexpected death of someone with epilepsy. These people are generally otherwise healthy and no other cause of death is found during an autopsy.
According to the Epilepsy Foundation, more that 1 in 1,000 people with epilepsy die each year from SUDEP and it is the leading cause of death in people with uncontrolled seizures.
If you watched the Disney Channel between 2011 and 2019, you may be familiar with Cameron Boyce who played Luke Ross on the “Jesse” and “Bunk’d” TV shows and also played Carlos in the “Descendants” movies. He died from SUDEP in 2019 at only 20 years old.
If you want to read about others who have passed away from SUDEP, click on over to the Epilepsy Foundation’s SUDEP Stories page.
Can someone with epilepsy exercise and/or play sports?
Yes, a person with epilepsy can, and should, play sports and exercise. We all know the importance of exercise on our overall health. Although we might think of exercise in terms of being physically fit, building muscles, or losing weight, we don’t usually think about the effects of exercise on our brain.
There have been several studies that have shown that exercise has a positive effect on depression, anxiety, ADHD, and more. The Epilepsy Foundation mentions that “research is showing that exercise and being physically fit may lessen risks of seizures!” But before you (or a loved one) jump in and start exercising or playing sports, certain precautions should be taken, depending on the activity. Here is a list of things to consider from the Epilepsy Foundation:
- Very rarely, exercise is a trigger for seizure activity. For the vast majority of people with epilepsy, the benefits of exercise far outweigh the risks.
- Common sense dictates that certain activities may need special accommodations or should be avoided.
- Most sports are safe for people with epilepsy to do, even if seizures aren’t fully controlled. However, the greater and more severe a person’s seizures, the greater the need for that person to limit or modify athletic activities.
- Using some simple safety precautions can help people stay active. For example,
-
- A woman with complex partial seizures enjoyed downhill skiing and just made sure she skied with her husband and used beginner or intermediate trails. People with frequent seizures or at risk for falls could use a harness on a ski lift.
- A man with rare tonic-clonic seizures roller blades every weekend and stays safe by wearing a helmet and knee and elbow pads. Even people without seizures should wear protective gear with many activities like this!
-
- Even if some activities need to be avoided, there are plenty of ways for people to stay active and exercise!
For further information about exercising and playing sports safely, visit this Epilepsy Foundation page. Assuming that you or your loved one is under a doctor’s care for seizures, get their input or advice on any sport or exercise that you are planning on doing.
What triggers seizures?
There are several commonly reported triggers such as these provided by the Epilepsy Foundation:
- Specific time of day or night
- Sleep deprivation – overtired, not sleeping well, not getting enough sleep
- At times of fevers or other illnesses
- Flashing bright lights or patterns
- Alcohol or drug use
- Stress
- Associated with menstrual cycle (women) or other hormonal changes
- Not eating well, low blood sugar
- Specific foods, excess caffeine or other products that may aggravate seizures
- Use of certain medications
To find out more about these triggers, visit the Epilepsy Foundation.
I don’t think we ever found a specific trigger for James’ seizures. They seemed to just happen at random times. Sometimes they seemed to occur when he was waking up, either from a full night’s sleep or from a nap. This was not always the case, though, so I’m not sure if would be considered a trigger or not.
Do people who have epilepsy also have developmental disabilities?
The answer to this question as it currently worded is not necessarily. The vast majority of people who have epilepsy or a seizure disorder do not have any developmental or intellectual disabilities.
If we were to ask the above question a bit differently, however, the answer would also be different. Do people who have developmental disabilities have a greater chance of having epilepsy? The answer to this question would be yes. According to Psychiatry Advisor, an estimated 1.8% of adults in the United States have epilepsy. For those that have an intellectual disability, the prevalence of epilepsy jumps to 22%.
What should I do if I see someone having a seizure?
If you’ve never witnessed someone having a seizure before, it can be a scary experience. When I was in 4th grade one of my teachers had a seizure during class. Almost 35 years later and I can still see her starting to stand up from her desk, let out this scream, raise her arm, pause for a second and then fall to the floor. Most of the class (including me) didn’t know what was happening to our teacher and just froze in our seats. A few of my classmates rushed to her while a couple of them ran to the school office to get help.
As you’ve learned previously, there are many different types of seizures. The actions you take to assist someone having a seizure is dependent on which type of seizure the person is having. Epilepsy Action in the UK put together the informative list below of dos and don’ts for each type of seizure.
- Tonic-clonic (convulsive) seizures
If you recall from the above, tonic-clonic seizures are generalized motor seizures, that occur in an individual with loss of consciousness. The tonic-clonic seizure consists of a tonic (bilateral increased tone, lasting seconds to minutes) and then a clonic (bilateral sustained rhythmic jerking) phase, typically in this order, however variations such as clonic-tonic-clonic and myoclonic-tonic-clonic can also occur.
-
-
- Do:
-
- Protect them from injury (remove harmful objects from nearby)
- Cushion their head
- Look for an epilepsy identity card or identity jewelry – it may give you information about their seizures and what to do
- Time how long the jerking lasts
- Aid breathing by gently placing them in the recovery position once the jerking has stopped (see picture)
- Stay with the them until they are fully recovered
- Be calmly reassuring
-
- Do:
-
-
-
- Don’t:
-
- Don’t restrain their movements
- Don’t put anything in their mouth
- Don’t try to move them unless they are in danger
- Don’t give them anything to eat or drink until they are fully recovered
- Don’t attempt to bring them round
-
- Don’t:
-
-
-
- Call 911 if:
-
- You know it is their first seizure or
- The jerking continues for more than five minutes or
- They have one tonic-clonic seizure after another without regaining consciousness between seizures or
- They are injured during the seizure or
- You believe they need urgent medical attention
-
- Call 911 if:
-
- Focal seizure
Someone having a focal seizure may not be aware of their surroundings or what they are doing. They may have unusual movements and behavior such as plucking at their clothes, smacking their lips, swallowing repeatedly or wandering around.
-
-
- Do:
-
- Guide them away from danger (such as roads or open water)
- Stay with them until recovery is complete
- Be calmly reassuring
- Explain anything that they may have missed
-
- Do:
-
-
-
- Don’t:
-
- Don’t restrain them
- Don’t act in a way that could frighten them, such as making abrupt movements or shouting at them
- Don’t assume they are aware of what is happening, or what has happened
- Don’t give them anything to eat or drink until they are fully recovered
- Don’t attempt to bring them round
-
- Don’t:
-
-
-
- Call for an ambulance if:
-
- You know it is their first seizure or
- The seizure continues for more than five minutes or
- They are injured during the seizure or
- You believe they need urgent medical attention
-
- Call for an ambulance if:
-
- Seizures in a wheelchair
Because James is unable to walk and is confined to a wheelchair for mobility, I was happy to see that Epilepsy Action included in their list what to do if someone in a wheelchair has a seizure.
-
-
- Do:
-
- Put the brakes on, to stop the chair from moving
- Let them remain seated in the chair during the seizure (unless they have a care plan which says to move them). Moving them could possibly lead to injuries for both you and them
- If they have a seatbelt or harness on, leave it fastened
- If they don’t have a seatbelt or harness, support them gently, so they don’t fall out of the chair
- Cushion their head and support it gently. A head rest, cushion or rolled up coat can be helpful
-
- Do:
-
The person’s care plan should give advice on what to do after the seizure has finished. For example, it should say if it is safe to move them from the wheelchair to put them in the recovery position.
-
-
- Don’t:
-
- Don’t restrain their movements
- Don’t put anything in their mouth
- Don’t give them anything to eat or drink until they are fully recovered
- Don’t attempt to bring them round
-
- Don’t:
-
Where can I find more information about epilepsy and seizures?
There is an abundance of information available on the Internet about epilepsy and seizures. I have included all of the resources that I referenced throughout this article in the list below. I have also included some additional resources that have good information about seizures and epilepsy. While it is good to do your own research, don’t forget to seek out a neurologist or qualified medical professional. He or she is the only one that can officially diagnose epilepsy and prescribe or recommend treatments.
Citizens United for Research in Epilepsy (CURE)
International League Against Epilepsy (ILAE)
Managing Epilepsy Well Network
US Centers for Disease Control and Prevention
